Treatment Advancements for Impaired Awareness of Hypoglycemia in Type 1 Diabetes
February 14, 2023
Innovations in Diabetes & Endocrinology | Winter 2023
It is estimated that 40 percent1 of individuals with Type 1 diabetes experience impaired awareness of hypoglycemia (IAH), defined as a diminished ability to perceive the onset of dangerously low blood glucose. As levels dip to 70 mg/dL, symptoms such as shakiness and irritability occur. At a threshold of 55 mg/dL or below, individuals may experience neuroglycopenic symptoms and become unable to stabilize their glucose levels without assistance. Unrecovered IAH can lead to seizures, coma, or death.
 Betul Hatipoglu, MD
Betul Hatipoglu, MDA complication of insulin therapy, IAH is often a barrier to attaining optimal glycemic control, explains Betul Hatipoglu, MD, medical director of the University Hospitals Diabetes and Metabolic Care Center. “Patients’ fear of IAH can become so pervasive that some individuals avoid hypoglycemia by keeping their blood sugar too high, which interferes with our interventions.”
Additionally, patients with Type 1 diabetes frequently do not remember that they have experienced hypoglycemic episodes, which account for up to 10 percent of deaths associated with Type 1 diabetes. “It is documented in the literature that patient reporting of IAH is less than 50 percent of real-life events,” says Dr. Hatipoglu. “Patients receiving insulin through pumps or injections should carry glucagon and have medical alerts on bracelets or driver’s licenses to prevent serious consequences.”
The expert team of clinicians and scientists within the UH Diabetes and Metabolic Care Center offers a multidisciplinary approach to monitoring and managing glucose levels. Here, Dr. Hatipoglu shares the progression of treatment options for patients who experience repeated episodes of IAH.
Continuous Glucose Monitoring
Today’s continuous glucose monitors (CGM) function in a closed-loop system with insulin pumps, suspending insulin delivery when blood sugar is low. “These systems are widely available and well-covered by insurance,” says Dr. Hatipoglu. “They have been shown in clinical trials to decrease time spent in severe hypoglycemia and improve overall control.” Audible alarms and app-enabled data reporting are helping patients self-recover from IAH episodes.
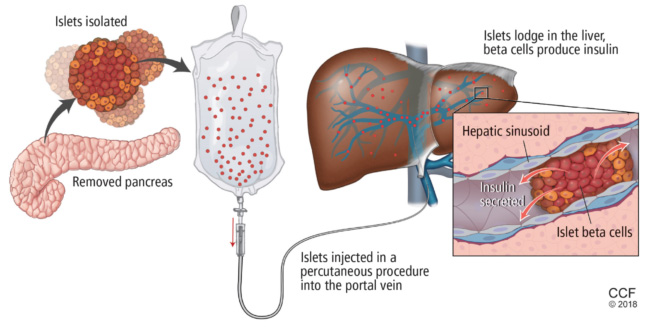 Reprinted with permission from: Rodeman K, Hatipoglu B. Beta-cell therapies for type 1 diabetes: Transplants and bionics. Cleve Clin J Med 2018; 85(12): 931-937; doi: 10.3949/ccjm.85a.17088. Copyright © 2023 Cleveland Clinic Foundation. All rights reserved.
Reprinted with permission from: Rodeman K, Hatipoglu B. Beta-cell therapies for type 1 diabetes: Transplants and bionics. Cleve Clin J Med 2018; 85(12): 931-937; doi: 10.3949/ccjm.85a.17088. Copyright © 2023 Cleveland Clinic Foundation. All rights reserved.Pancreas Transplantation
“If patients are having difficulty managing their diabetes appropriately due to hypoglycemia and hypoglycemic unawareness, it is time to consider pancreatic transplant,” says Dr. Hatipoglu. “Someone could be walking around with an A1C of 9 or above to avoid hypoglycemia, but that is not appropriate control and leads to detrimental results — including retinopathy, nephropathy, neuropathy or other complications of diabetes.”
Available since the 1960s, pancreatic transplant surgical techniques, outcomes and survivability have improved tremendously over the past decades. The whole-organ transplant procedure requires matching each patient to a deceased donor pancreas. However, patients who are fortunate to receive transplantation can achieve complete insulin independence, explains Dr. Hatipoglu. “One-year survival and function of a pancreas transplant is close to 100 percent in many centers, five-year survival is close to 70 percent, and 10-year survival is around 50 percent.” She adds that well-equipped medical centers such as University Hospitals can evaluate patients to determine whether they are appropriate candidates and weigh benefits against the risks of organ transplantation, including infection or bleeding and the need for lifelong immunosuppressive drug therapy.
Islet Cell Transplantation
Islets are clusters of hormone-producing cells that are extracted from a deceased donor pancreas. The islet cells are purified and infused through the portal vein directly into the liver. Dr. Hatipoglu began researching the novel therapy in the early 2000s, serving as medical director for the pancreas and islet cell transplant program at the University of Illinois at Chicago for nearly eight years.
“Beta cells within the islet begin to produce insulin, effectively curing a person of diabetes,” she says. While the outpatient procedure carries fewer risks than whole organ transplantation, patients still require lifelong immunosuppressive medications. Additionally, patients may require a subsequent infusion, increasing the demand on pancreas donor banks.
In April 2021, the Federal Drug Administration approved islet cell transplantation for patients with brittle Type 1 diabetes who do not respond to conventional therapies. Currently, patients must travel to a limited number of centers across the United States to receive donor islet cells. Dr. Hatipoglu and her team work to guide patients through the approval process.
“Our hope is that this treatment option will soon become more widely available for diabetic patients who are ineligible for pancreas transplantation,” she says. “I am excited about these advancements and thrilled to be able to offer patients the best possible treatment options.”
For more information, contact Betul Hatipoglu, MD, at Betul.Hatipoglu@UHhospitals.org.
1 International Hypoglycemia Study Group. Diabetes Care. 2015;38(8):1583-1591. Agiostratidou G, et al. Diabetes Care. 2017;40(12):1622-1630. Cryer PE. Am J Med. 2011;124(11):993-996.
Contributing Expert:
Betul Hatipoglu, MD
Medical Director
University Hospitals Diabetes and Metabolic Care Center
Vice Chair, UH System Clinical Affairs
Mary B. Lee Chair in Adult Endocrinology
University Hospitals Cleveland Medical Center
Professor, Case Western Reserve University School of Medicine


