Overcoming Barriers for Patients with Type 1 Diabetes
November 06, 2022
Innovations in Diabetes & Endocrinology | Fall 2022
Search insulin on the popular crowdfunding site GoFundMe, and scroll through pages of individuals resorting to online pleas for the medication, insulin pumps and supplies required to control blood sugar. As part of her postdoctoral fellowship at the University of Utah, Julia Blanchette, PhD, RN, BC-ADM, CDCES, a Diabetes Nurse Scientist within the University Hospitals Diabetes & Obesity Center, was on a team that analyzed numerous profiles of GoFundMe posters seeking support.
 Julia Blanchette, PhD, RN, BC-ADM, CDCES
Julia Blanchette, PhD, RN, BC-ADM, CDCES“People are choosing this route because of substantial costs and health insurance inadequacies, but these avenues aren’t sustainable ways to manage their condition,” she says. “What can diabetes care and education specialists and providers do to ensure that marginalized individuals are better supported?”
At particular risk are emerging adults. Approximately half of type 1 diabetes is diagnosed in childhood. Emerging adults often struggle to navigate changes in their care delivery and the financial burden of lifelong treatment.
“Higher levels of financial stress contribute negatively to A1C and diabetes-related quality of life,” says Dr. Blanchette. “We see lapses in accessing health services during the transition to adulthood, resulting in suboptimal self-management outcomes and increased risk of hospitalizations related to hyper- or hypoglycemia.”
To tackle gaps in diabetes self-management education and support (DSMES) and care, Dr. Blanchette collaborated with a community advisory board to develop a financial and health insurance literacy toolkit. Young adults with type 1 diabetes from diverse backgrounds led a 10-part series of brief, informative videos aimed at building health insurance and financial literacy, gaining skills to navigate the complex healthcare system and managing the resulting mental health burden.
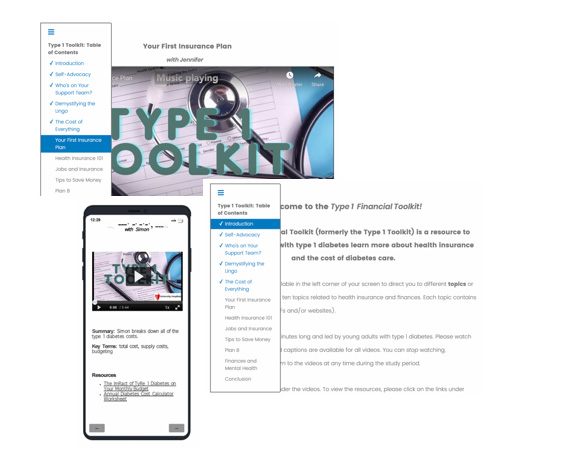 Caption: Mobile and web browser views of the financial and health insurance toolkit.
Caption: Mobile and web browser views of the financial and health insurance toolkit.“Part of becoming an adult is learning how to balance finances with the rest of your life, but those with type 1 diabetes have the added burden of diabetes costs,” she says. The videos include a variety of perspectives from young adults with type 1 diabetes at different stages of life sharing their journey, addressing options for health insurance and suggesting community resources.
Next, Dr. Blanchette piloted the videos with 40 young adults with type 1 diabetes at the University of Utah and followed them for several months. “We found that the educational intervention improved participants’ health insurance literacy, financial stress, diabetes management and quality of life over time,” she says.
Dr. Blanchette’s next step is to tailor the toolkit to meet the needs of racially and ethnically diverse young adults with type 1 diabetes in the Medicaid system. “There are a lot of factors to consider. Do they have transportation? A safe living environment? Access to food?” she asks. “For those who qualify for benefits, there are still social determinants of health that can make it difficult to navigate the Medicaid system or prioritize diabetes self-management.”
Continuous Glucose Monitoring
As of September, the Ohio Department of Medicaid is now covering continuous glucose monitoring (CGM) for individuals with type 1 or type 2 diabetes if their HbA1c is above 7.0 percent. CGM devices measure glucose levels every few minutes and provide real-time feedback on the impact of medications, food, physical activity and stress.
“University Hospitals partnered with local health officials to invite patients who qualify to wear a CGM free of charge,” says Blanchette. “However, you can’t just make an appointment and get started. The device is one part of a comprehensive treatment plan.” A quality improvement initiative within the UH Diabetes & Obesity Center and the system’s population health department is identifying individuals with elevated A1C who could benefit from the program. Innovation support services are also offered, including ambulatory pharmacies, home delivery and virtual visits for setup education. “We started with the highest-risk patients who have kidney or cardiovascular complications. Once we reached out to those patients, we targeted Medicaid patients who have an A1c over 7.0 percent. Our goal is to start the most vulnerable on CGM therapy and establish follow-up care that they might not otherwise receive.”
For more information, contact Julia Blanchette at Julia.Blanchette@UHhospitals.com.
Contributing Expert:
Julia Blanchette, PhD, RN, BC-ADM, CDCES
Diabetes Nurse Scientist
University Hospitals Cleveland Medical Center
Clinical Assistant Professor
Case Western Reserve University School of Medicine


