Research, Outreach at UH Rainbow Addressing Disparities, Equity and Social Determinants of Health
June 22, 2021

Several projects under way to help improve outcomes for vulnerable groups
Innovations in Pediatrics | Summer 2021
Projects across UH Rainbow Babies & Children’s Hospital are addressing the unique needs of vulnerable populations and the role of social determinants of health in driving outcomes. Some projects involve collecting data on disparities and equity that perhaps hasn’t been collected before, while others involve facilitating care for those who could benefit from some extra effort, such as newly arrived immigrants learning to navigate the healthcare system in the U.S. for the first time.
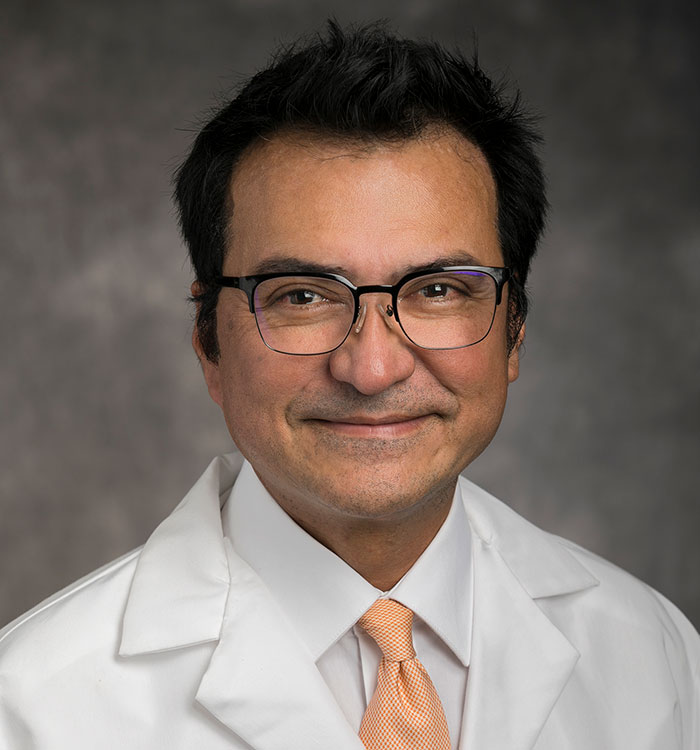 Charles Macias, MD, MPH
Charles Macias, MD, MPHUH Rainbow, for example, is one of a handful of American children’s hospitals participating in workgroup known as Patient Harm Associated with Race and Ethnicity (PHARE) through Solutions for Patient Safety (SPS). It seeks to quantify whether there are disparities in hospital-acquired conditions such as central line associated bloodstream infections and surgical site infections by race and ethnicity.
“Being able to look at race and ethnicity is so critical for us to understand how and for whom we are achieving intended outcomes,” says Charles Macias, MD, MPH, Division Chief of Pediatric Emergency Medicine and Chief Quality Officer at UH Rainbow. “Is there really something genetically involved or, much more likely, is it a disparity in barriers to high quality care? We need to understand whether other social determinants are preventing our healthcare system from getting to the outcomes we're trying to achieve.”
Data like this has traditionally been quite hard to come by, Dr. Macias says. In a previous SPS study of children’s hospitals, for example, only 20 percent of survey respondents reported comparing readmission rates between racial and ethnic groups. But things are changing now, he says.
“Children's hospitals are awakening,” he says. ”We don't think of ourselves as delivering variable care when we're delivering good care to all children. But there’s a difference between equality and equity. High quality care delivery requires that we tailor our care to the needs of the family and the child. It should recognize the social determinants and the barriers that are unique to certain groups of children.”
Beyond the PHARE study, Dr. Macias and his UH Rainbow colleagues are also gathering data on disparities and equity among pediatric patients with asthma, sepsis and those receiving vaccines – and seeking solutions to mitigate them.
Pediatric intensivist Katherine Slain, DO, Director of the Pediatric Critical Care Medicine Fellowship Program at UH Rainbow, is also addressing disparity and equity issues in her research and clinical work.
“Even though intuitively, it seems that vulnerable children and vulnerable families are going to have worse ICU stays, worse outcomes after ICU stays, very few researchers have actually taken the time to do a deep dive to see if that's really true,” she says.
To remedy this, Dr. Slain is working with a large data set involving inputs from 50 children’s hospitals nationwide, looking at the relationship between PICU outcomes and social determinants of health.
“I am currently using large multicenter datasets to investigate differences in hospital outcomes based on different social factors,” she says. “Are there differences in illness severity, PICU admission rates, hospital length of stay, or mortality in children of different races, different incomes or different insurance?
Initial results show that African-American children have a longer length of stay in the PICU for some conditions, such as traumatic brain injury and sepsis, but not for others, such as pneumonia or bronchiolitis, Dr. Slain says. “Differences in health outcomes between children of different races and different socioeconomic status is unacceptable. We must take this information and change the way we practice medicine to ensure all our children are receiving equitable care.”
She is currently designing multiple interventions that seek to mitigate differences in outcomes, including one planned with teachers and schools. One already under way involves an in-depth interview with patient families at the time of PICU admission.
“It's a 30-minute interview to really try to identify how the PICU stay is impacting the family and not just the health of the child,” she says. “We ask, ‘What kind of resources do you have? What kind of help do you have at home? Are you having issues with childcare or are you having issues with transportation? Are you having issues getting food? Are you able to be at the bedside? If not, why not? How can we help you take care of your child and family while here at UH Rainbow?’ We're recruiting a hundred different families and hope eventually to start to identify patterns of what our families actually need when their children are admitted to the PICU.”
On another front, UH Rainbow residents and fellows in developmental and behavioral pediatrics are working with one extremely vulnerable population to help improve outcomes – immigrants who are newly arrived to the metropolitan Cleveland area.
“We've had a really nice partnership for just the last couple of years now with the United States Committee for Refugees and Immigrants,” says Marie Clark, MD, MPH, a developmental and behavioral pediatrician at UH Rainbow. “We reached out to see what we could do to support that population. One of the things that they felt would be really useful is kind of healthcare curriculum for the refugees. When they come here, the U. S. healthcare system is completely foreign to them. So what we’ve done is introduce them to that and help all of them to understand medical care here, including diet and hygiene and recommendations around that.”
Jasmine Wilaisakditipakorn, MD, a developmental-behavioral fellow at UH Rainbow, received a $10,000 grant from the American Academy of Pediatrics’ Community Access to Child Health fund to support this work. She and her fellow residents and fellows have been conducting educational Zoom sessions with immigrant families for the past several months. They’ve also produced videos and a handout families can refer to with their questions.
Dr. Clark says she and the residents and fellows plan to use this project to better understand how to communicate and care for vulnerable groups. They’re planning focus groups with immigrant families on what they’ve learned, as well as a study of residents and fellows to see how the project has changed their knowledge and understanding about how to work with this vulnerable population.
“We’ve created a long-standing product that the U.S. Committee for Refugees and Immigrants will now have available to use with families,” Dr. Clark says. “But we can also use this project to improve how we care for this vulnerable group.”
For more information on the different projects at UH Rainbow Babies & Children’s Hospital addressing vulnerable populations, please email Peds.Innovations@UHhospitals.org.
Contributing Experts:
Charles Macias, MD, MPH
Division Chief, Pediatric Emergency Medicine
Chief Quality Officer
UH Rainbow Babies & Children's Hospital
Clinical Associate Professor
Case Western Reserve University School of Medicine
Katherine Slain, DO
Program Director, Pediatric Critical Care Medicine
Director, Pediatric Critical Care Medicine Fellowship Program
UH Rainbow Babies & Children's Hospital
Assistant Professor
Case Western Reserve University School of Medicine
Marie Clark, MD, MPH
Developmental Behavioral Pediatrics & Psychology
UH Rainbow Babies & Children's Hospital
Assistant Professor
Case Western Reserve University School of Medicine