Researchers Develop Skeletal Maturity System for the Digital Age
January 04, 2021
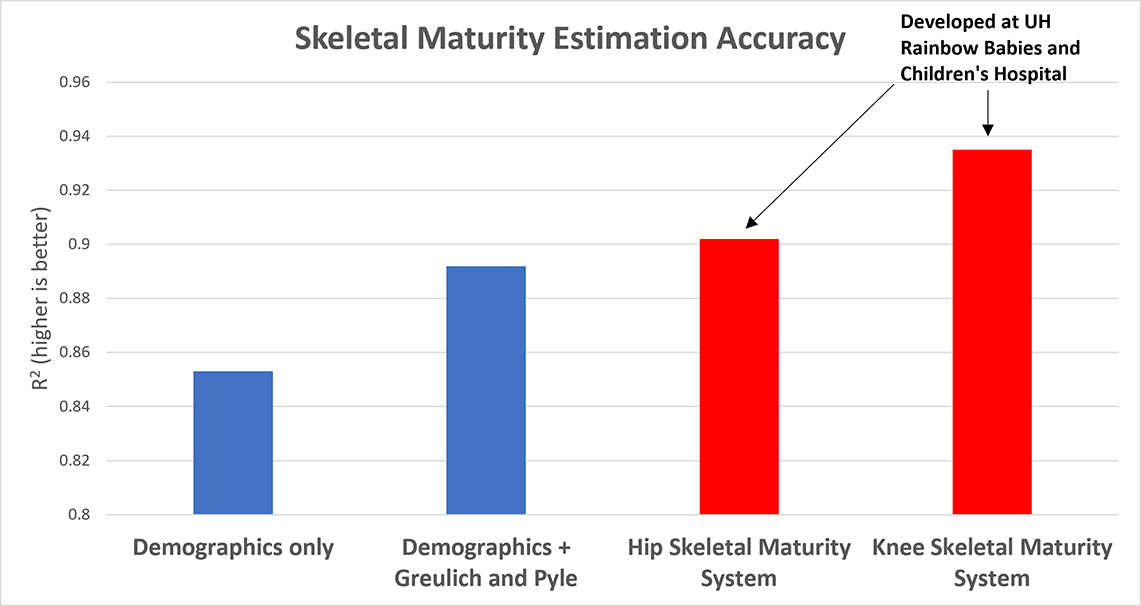
Recent studies using system show comparable results to Greulich and Pyle standard
Innovations in Orthopaedics | Winter 2021
 Raymond Liu, MD
Raymond Liu, MDPhysicians and radiologists have used the Greulich and Pyle Atlas to measure bone age in children for 60 years. While many still refer to the Atlas to aid diagnoses, the method has its limitations. In an era where advanced technology can generate precise analyses of vast datasets in minutes, isn’t there a better way?
Using modern computing, advanced mathematics and priceless historical archives, three University Hospitals physicians — Raymond Liu, MD, Victor M. Goldberg Endowed Chair in Orthopedics at UH Cleveland Medical Center and a pediatric orthopedic surgeon at UH Rainbow Babies & Children’s Hospital, and Associate Professor at Case Western Reserve University School of Medicine, orthopedic surgery residents Ryan Furdock, MD, and Alexander Benedick, MD — have developed a digitized skeletal maturity system that may deliver more accurate results than the Greulich and Pyle standard.
“A physician seeing patients every 15 minutes doesn’t have time to look up what they need in the Atlas,” Dr. Liu says. “We hope to mobile-optimize our system so physicians can open a common orthopaedic app, go to the skeletal maturity section, and proceed through a few steps to determine bone age.”
MEETING THE NEED FOR BETTER MEASUREMENTS
An accurate measurement that estimates remaining skeletal growth is crucial when treating children with congenital or acquired limb-length inequalities and other conditions. “In a procedure such as hemiepiphysiodesis, for example, where we stop one side from growing, when a child is close to maturity, we need to know whether he or she has enough growth left for the surgery to work,” Dr. Liu says. “This information will be valuable in those cases. ”The new system may also help treat scoliosis, which often progresses around puberty but generally does not worsen after bone growth ends. “We need to know when bone growth is going to stop, and it’s hard to estimate from looking at the spine,” he says. “Our hip system may potentially help us determine which patients will benefit from bracing, need longer periods of observation or benefit from certain surgical approaches such as tethering.”
Slipped capital femoral epiphysis (SCFE) is another area of focus. SCFE usually occurs on only one side of the hip; however, about 40 percent of patients will develop SCFE on both sides. “Because patients who are less skeletally mature are more likely to develop SCFE on both sides, we can use our hip system to better stratify risk and potentially perform surgery to stop slippage before it happens,” Dr. Furdock says.
ADVANCED STATISTICAL METHODS HELP IMPROVE ACCURACY
To design the skeletal maturity system, Dr. Furdock dug into radiographic data found at Case Western Reserve University’s Bolton-Brush Growth Study Center, the world’s most extensive source of longitudinal human growth data. The Brush Inquiry, which is part of the collection, was conducted by professor T. Wingate Todd from 1926 to 1942 to examine human mental and physical growth and development.
Among other data, Todd took X-rays of the skull and entire left side of the body of all study participants, as often as every three months to every year. Such a vast collection of images helped Dr. Furdock test theories as well as establish a gold standard.
“When building this type of system, you need a complete set of data to calibrate that system,” Dr. Furdock says. “The Bolton-Brush collection gives us the data to help build the equations that allow the system to make predictions.”
The standards determined by Greulich and Pyle use hand and wrist X-rays. To reduce the amount of imaging required of young patients, Drs. Liu and Furdock based their standards on knee and hip images — images patients often already have on file.
When evaluating the hip, Dr. Furdock used 14 X-ray measurements. When evaluating the knee, Dr. Benedick used a separate set of 14 X-ray measurements. Using a stepwise multivariate linear regression method, researchers can identify which of those 14 hip or knee measurements are most important. This helps improve accuracy of the system and allows physicians to get an accurate measurement in fewer steps.
Recent studies using the new system have shown comparable results compared to the Greulich and Pyle standard using hip images. Knee images generate above-standard accuracy.
USING MODERN TECHNOLOGY TO ITS FULLEST
Technology barely imagined 50 years ago will help bring the skeletal maturity system to physicians’ offices via a device they already have on hand: their smartphone. Dr. Furdock says he’s testing an app version of the system with five School of Medicine students, five University Hospitals orthopaedic residents, and five attending physicians at UH Rainbow Babies & Children’s Hospital.
“We’re using technology to create something practical and useful,” Dr. Liu says. “Our goal over the next year is to work with colleagues around the country to get these parameters onto apps. It’s not fancy technology, but it’s so critically important from a practical and clinical perspective.”
For information about the system, contact Raymond Liu, MD at Raymond.Liu@uhhospitals.org or the UH Department of Orthopaedics at 216-553-1783.
Related publications:
- Benedick A, Knapik DM, Duren DL, Sanders JO, Cooperman DR, Liu RW. Systematic isolation of key parameters for estimating skeletal maturity on knee radiographs. Accepted for Publication by Journal of Bone & Joint Surgery 11/27/20.
- Furdock RJ, Benedick A, Nelson G, Li D, Cooperman DR, Sanders JO, Liu RW. Systematic isolation of key parameters for estimating skeletal maturity on AP hip radiographs. Submitted to Journal of Bone & Joint Surgery 12/12/20.
- Nelson GB, Knapik DM, Janes JL, Liu RW. Greater Trochanter Height: A Quantitative Predictor of Skeletal Maturity. J Pediatr Orthop. Published online Dec 2020. doi:10.1097/BPO.0000000000001724.
- Knapik DM, Sanders JO, Gilmore A, Weber DR, Cooperman DR, Liu RW. A quantitative method for the radiological assessment of skeletal maturity using the distal femur. Bone Jt J. 2018;100B(8):1106-1111.


