Algorithm Helps Physicians Better Detect Concerning Pancreatic Cysts
October 19, 2020
Automated process streamlines and standardizes diagnosis and treatment
Innovations in Digestive Health | Fall 2020
 Jordan Winter, MD
Jordan Winter, MD Jeffrey Hardacre MD
Jeffrey Hardacre MDPancreatic cysts usually aren’t cause for concern. But when they are, early detection and treatment can prevent these cysts from progressing to pancreatic cancer.
Because many patients learn about pancreatic cysts by chance—they appeared on a CT scan or an MRI for an unrelated condition — their presence often goes unnoticed. While benign cysts usually don’t require further treatment, cancerous or precancerous cysts require ongoing surveillance or surgery.
“It’s a challenge for radiologists at hospitals and health systems nationwide: when they identify incidental findings, who is responsible for appropriate follow up and management of those findings?” says Jordan Winter, MD, Chief of Surgical Oncology, University Hospitals Cleveland Medical Center, and Professor of Surgery, Case Western Reserve University School of Medicine. “Our pancreatic surgeons want to take responsibility for our disease domain. The worst thing that can happen is these cysts get lost to follow up.”
To ensure these patients receive proper and faster notification, and — when necessary — more immediate treatment, University Hospitals Digestive Health Institute developed a detection and notification process for findings of concern. The process starts in radiology: software identifies images containing certain trigger words and flags those images for review.
Flagged images are reviewed every week by Dr. Winter or Jeffrey Hardacre, MD, Chair, Surgical Oncology Quality Committee, UH Cleveland Medical Center and Professor of Surgery, School of Medicine. Out of 60 to 75 scans per week, Dr. Winter and Dr. Hardacre may identify 10 to 12 scans that require next-level surveillance, which starts with a call to the primary care or treating physician. Between one to three patients per week are appropriate for surgical consultation.
“The automatic alert process we’ve developed is a work in progress, but we have improved communication between our team and the primary care physicians,” Dr. Hardacre says.
THE TREATMENT ALGORITHM
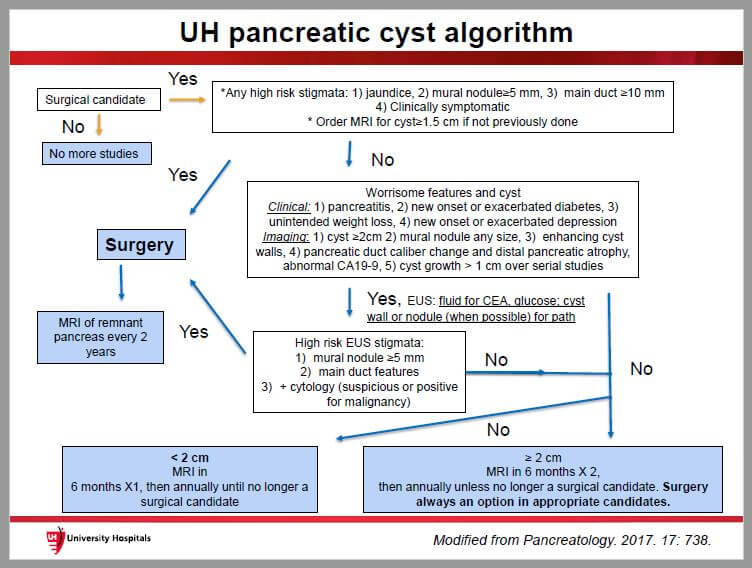
To streamline and standardize diagnosis and treatment, Dr. Winter and team developed a pancreatic cyst algorithm for concerning findings. The current version of the algorithm has been in place for about a year and helps physicians determine the proper path to treatment.
“We also rely on the cyst clinic and we present lesions with particular features or size concerns to our weekly multidisciplinary review,” Dr. Winter adds. “It’s a multidisciplinary process that uses shared decision-making to manage these patients according to best practices.”
In an article for Translational Cancer Research, Nathan Berger, MD, a member of the GI Cancer Genetics Program at the Case Comprehensive Cancer Center and Professor of Medicine, Biochemistry, Oncology, Genetics and Genome Sciences at the School of Medicine, noted that a Mayo Clinic study that found the five-year risk for developing pancreatic cancer was 49.7 percent in high-risk groups (obstructive jaundice, cystic lesions in pancreas head, solid components within cysts, thickened or enhancing cyst wall, or main duct dilatation >10 mm), while the risk for those with “worrisome features” (pancreatitis without other causes, cysts >3 cm, thickened walls, main duct dilatation 5–9 mm, mural nodules, lymphadenopathy, abrupt change in duct dilatation with distal pancreatic atrophy) was 5.1 percent.1
It will take time before Dr. Winter and Dr. Hardacre have data to show whether their process helps lower the cancer rate. However, early benefits are encouraging. “We’re not only improving the notification process and the time to getting a biopsy or a referral, we’re improving time to treatment,” Dr. Winter says.
Important Links & Numbers
Refer a Patient: 216-844-3951
Transfer Referral Center: 800-421-9199


