UH Rainbow's Martin Bocks, MD and Colleagues Awarded $25,000 from the PediaVascular Pitch Competition at the Pediatric Interventional Cardiac Symposium
November 04, 2019

“No device left behind” is the mantra behind groundbreaking work to develop a bioresorbable occluder for transcatheter closure of atrial septal defects. Martin Bocks, MD, University Hospitals Rainbow Babies & Children's Hospital Cath Lab Director, and a team of biomedical engineers at Georgia Tech were awarded $25,000 from the PediaVascular Pitch Competition at the Pediatric Interventional Cardiac Symposium for their novel prototype that utilizes a technologically advanced, fully-bioresorbable material called poly-glycerol dodecanoate (PGD) to close holes in the heart. The funds will be used to develop the final prototype before proceeding with pre-FDA testing.
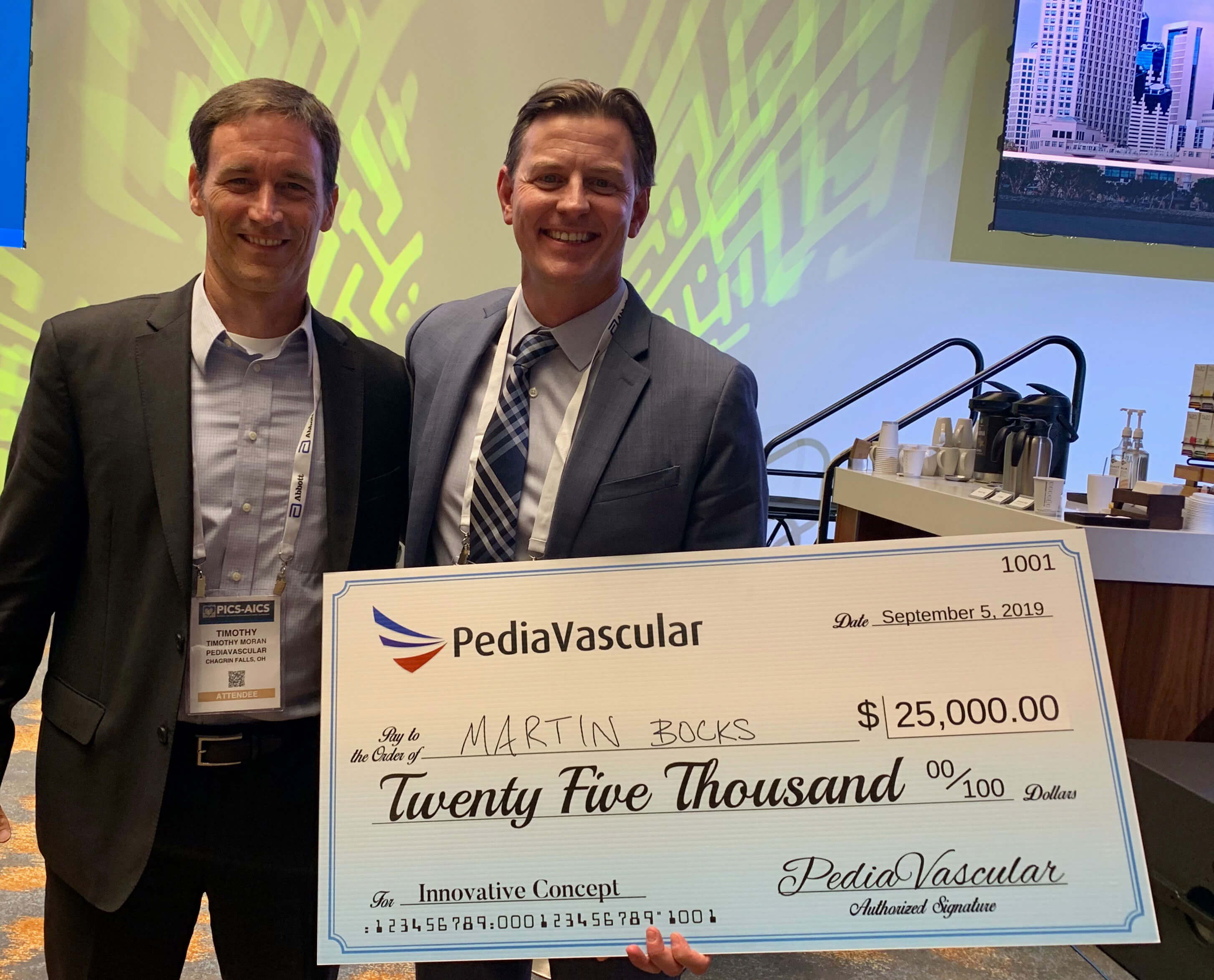 Martin Bocks, MD and Tim Moran, Founder and President of PediaVascular .
Martin Bocks, MD and Tim Moran, Founder and President of PediaVascular .Atrial septal defects, or ASDs, are one of the most common diagnosed congenital heart defects (CHD), accounting for nearly 5-10 percent of CHD in children and 30-40 percent of CHD in adults. The devices currently marketed for percutaneous closure, successful in their use, have short and long-term limitations Dr. Bocks is hopeful his novel device can address. In particular, the bioresorbable occluder will be soft, with characteristics of the surrounding heart tissue, replacing the current rigid frame adjacent to healthy heart tissue. This should prevent the device from potentially injuring the heart or causing arrhythmias.
“What is most exciting about this device is its ability to completely resorb at a controlled rate, allowing for the device to be replaced over time by the body’s own heart cells,” says Dr. Bocks. “This would be the first customizable cardiac device, which really is and should be the future of medical implants as opposed to the one-size-fits-all approach we have used for years.”
Using PGD will allow interventional cardiologists to close holes in the heart but not make access to the left side of the heart difficult or impossible, should the patient need a procedure when they are older to treat conditions such as atrial fibrillation or mitral valve disease. Dr. Bocks is excited about the potential to 3D print these devices and make them in shapes and sizes specific to a patient’s heart dimensions.
The project team, led by Dr. Bocks, plans to finalize the prototype in 2020.
To contact the Congenital Heart Collaborative or Dr. Martin Bocks, call 216-714-8358.


