Basic & Translational Leukemia Research
Translating Basic Research to Offer Advanced, Responsive and Effective Care
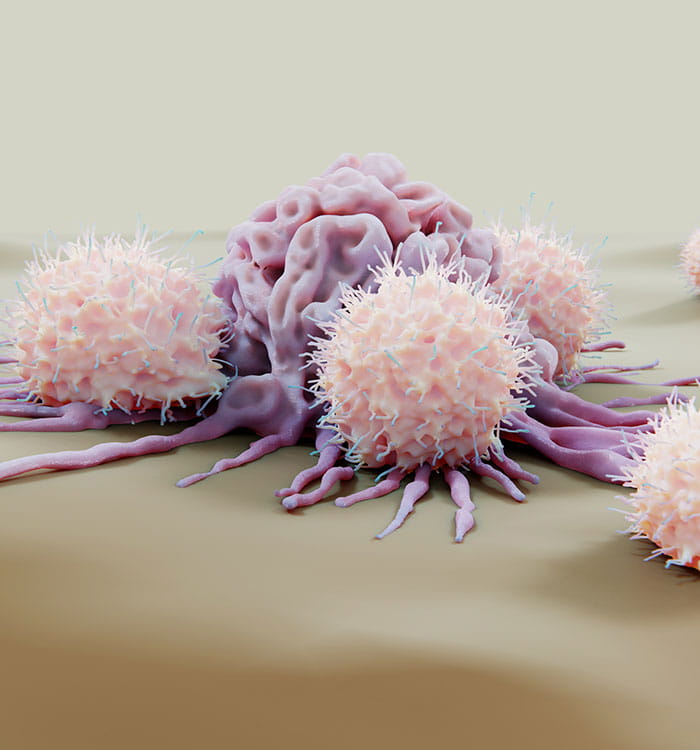
The complexity of leukemia, a group of cancers of the blood and blood-forming tissues of the body, can make it hard to treat. Every patient’s disease is unique with a multitude of underlying biologic, molecular and genetic factors driving its progression.
Physician-scientists at the UH Seidman Cancer Center translate basic research findings to clinical practice to provide patients with the most advanced, responsive, and effective care, advancing the precision of targeted drug treatment and immunotherapy. Throughout their work, they strive to better understand the pathogenesis of leukemia, pinpoint the genetic and epigenetic changes that contribute to the proliferation and spread of cancer cells, and identify biological pathways enhance to enhance to make tumors more responsive to treatment. Their aim is to develop new, less toxic treatments, that are better tolerated by even the most medically fragile patients, while also developing strategies for treatment-resistant cancers and relapsed leukemia.
For instance, large adult and pediatric Acute Myeloid Leukemia (AML) studies are underway to identify genetic biomarkers to serve as drug targets and help predict outcomes. Other research examines what factors induce the toxic side effects of chemotherapy or make tumors resistant to drug treatment. Additional research outlines the biology of relapsed leukemia and the underpinnings of relapsed leukemia. Researchers also seek to reduce potential treatment complications such as graft-versus-host disease following stem cell or bone marrow transplantation.
Throughout their work, researchers expand the study of small molecule inhibitors for targeted therapies, and develop and test combination treatment regimens, expanding the use of immunotherapy, NK cell and CAR T-cell therapy, to leverage discovery and innovation, and to improve clinical outcomes and disease prognosis.
Researchers Study Relapse Prevention Mode for Acute Lymphoblastic Leukemia Patients
A UH Seidman Cancer Center team led by Leland Metheny, MD, reported on a multicenter Phase I study of post-transplant low-dose intouzumab ozogamicin (INO) to prevent relapse of Acute Lymphoblastic Leukemia (ALL). INO is an anti-CD22 monoclonal antibody bound to calicheamicin and approved to treat relapsed ALL. The primary objective of the trial was to define a post-allogeneic transplant maximum tolerated dose (MTD) of INO. Trial results show that INO at doses of 0.3, 0.4, 0.5 and 0.6mg/m2 was well tolerated and that 0.6 mg/m2 is the MTD. Thrombocytopenia may be the dose-limiting toxicity. The researchers say that the low observed relapse rate and favorable safety profile justify investigating low-dose INO as maintenance therapy after alloHCT in a Phase II trial.
 NK Therapeutics Offer New Approach for Treating Blood and Colorectal Cancers
NK Therapeutics Offer New Approach for Treating Blood and Colorectal Cancers
Researchers at the UH Seidman Cancer Center led by David Wald, MD, PhD, recently completed a Phase I clinical trial testing the use of natural killer, or NK cells, in patients with either colorectal cancer or blood cancer. Although results are yet to be published, the new method which expands and activates large numbers of NK appears to be more effective against blood cancers than against solid tumors. Several follow-up trials are planned. Long term, if successful, this new method, NK cell adoptive therapy, which is licensed commercially through a partnership between Case Western Reserve University and the Australian company Chimeric Therapeutics, could make NK technology available to more cancer patients, including those with leukemia.
CAR T-Cells Produced Onsite at UH Seidman Cancer Center Yield High Remission Rates in B-cell Malignancies
 Research at the UH Seidman Cancer Center shows newly designed chimeric antigen receptor CAR T-cells targeting the CD19 antigen are especially effective in treating adults and children with B-cell malignancies when produced onsite and administered more quickly to patients than commercially produced CAR T-cell products. At the UH Seidman Cancer Center, CAR T-cells are produced in the Wesley Center for Immunotherapy.
Research at the UH Seidman Cancer Center shows newly designed chimeric antigen receptor CAR T-cells targeting the CD19 antigen are especially effective in treating adults and children with B-cell malignancies when produced onsite and administered more quickly to patients than commercially produced CAR T-cell products. At the UH Seidman Cancer Center, CAR T-cells are produced in the Wesley Center for Immunotherapy.
Preliminary findings published in the journal Nature Communications described two Phase I clinical trials of CAR19 T-cells used to treat patients with relapsed/refractory pediatric B-cell Acute Lymphocytic Leukemia (ALL) or adult B-cell Lymphoma. In the mouse xenograft experiments, fresh CAR19 T-cells produced in the Wesley Center for Immunotherapy were shown to provide an advantage over cryopreserved cells more commonly used in CAR T applications.
According to the research, administration of fresh CAR19 T-cells yielded significantly lower tumor burden as compared to dose-matched frozen CAR19 T-cells on study days 11 and 13. On study days 21 and 28, tumors were similarly and potently rejected by both fresh and frozen cell-treated groups. However, fresh cells reduced the tumor burden sooner by eight days, and immediately started reducing the tumor burden, while frozen CAR19 T-cells first permitted tumor growth before controlling growth.


