Division of Thoracic and Esophageal Surgery Provides Specialized Services for Better Patient Outcomes
University Hospitals Division of Thoracic and Esophageal Surgery has been a leader in developing less-invasive techniques using smaller incisions and conservative resections to minimize complications, shorten hospital stays and quicken recovery.
Several examples of the novel approaches available at University Hospitals include:

Video-Assisted Thoracic Surgery (VATS)
VATS is a minimally invasive alternative for diagnosis and treatment of patients with lung cancer. VATS involves smaller incisions without large muscle or rib division and no rib spreading. With results identical to those seen when using the traditional open technique, patients benefit from less post procedure pain, fewer complications, lower transfusion requirements, less tissue loss and scarring and faster return to normal activities.
Robotic Thoracic Surgery
Instead of performing the procedure at the operating room table, a UH surgeon is seated at the robot console and remotely controls robotic arms that perform the operation. The robotic camera provides 3-D visualization and the robotic arms allow for fine movements in tight spaces such as the center of the chest. Length of stay, complication and cure rates are similar to results with VATS.
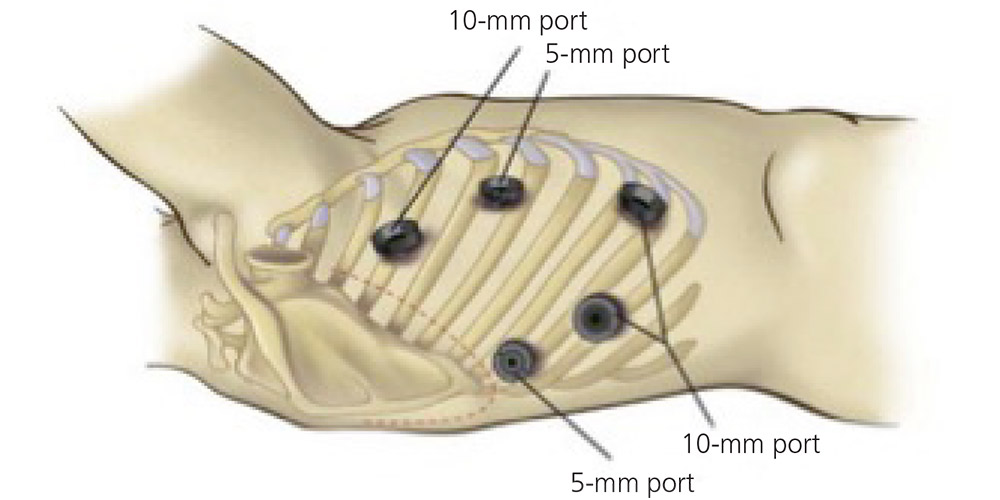
Minimally Invasive Esophagectomy
Surgeons at UH Cleveland Medical Center are one of a select number of teams nationally performing minimally invasive esophagectomy for patients with esophageal cancer, and the first site in Northeast Ohio to perform this procedure. Most patients experience less pain, fewer wound complications, less blood loss and a quicker return to normal activity. Outcomes are similar or better to traditional open esophagectomy. Robotic esophagectomy is also performed in a similar minimally invasive fashion.

Proton Therapy for Thoracic Tumors
Proton therapy is uniquely suited for treatment of tumors of the chest. This targeted therapy allows for potentially curative radiation doses to be administered to tumors near the heart and spinal cord, while sparing those vital structures from potentially damaging radiation.
University Hospitals Seidman Cancer Center has the only proton therapy center in Northern Ohio.
Proton therapy is an external beam radiation similar to conventional high-energy X-rays, but the protons are larger and doses are delivered in a more targeted manner. By changing the energy of the proton beam, radiation oncologists can tailor the proton dose to the specific depth and shape of the tumor, while greatly reducing the dose to surrounding healthy tissue. When used for specific tumors, proton therapy can decrease side effects, which may result in a better quality of life during treatment, and has the potential to reduce the risk for developing radiation-induced secondary cancers decades after treatment.
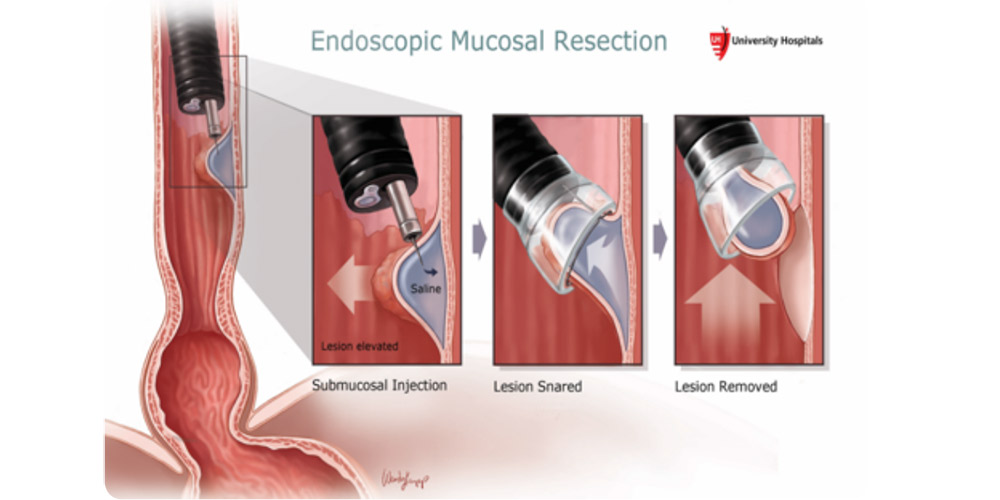
Endoscopic Mucosal Resection (EMR) and Endoscopic Mucosal Dissection (ESD)
Gastroenterologists of University Hospitals Digestive Health Institute are national leaders in surveillance of Barrett’s esophagus and endoscopic techniques such as endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD). These techniques allow for treatment of early esophageal cancers by endoscopic resection without the need for esophagectomy. Barrett’s can be ablated with either radiofrequency or cryotherapy, and the patients are closely followed for any potential recurrence.


