Lipid Screenings in Children and Adolescents

Ischemic cardiovascular disease (CVD), including coronary heart disease and stroke, is characterized by reduced blood flow to the heart. It is the most common cause of mortality in the world. With rising rates of obesity, type 2 diabetes, atherosclerosis and other known risk factors for CVD, it is increasingly important to identify at-risk populations to prevent the development of future CVD events with effective management.
In 2011, the National Heart, Lung, and Blood Institute (NHLBI) Expert Panel published updated guidelines for cardiovascular health and CVD risk reduction in youth. One of the main points of these guidelines is the strong recommendation for universal lipid screening for patients who are between 9 and 11 years old and a second universal screening when patients are between 17 and 21 years old.
However, targeted (selective) screening should be done starting at 2 years old if the patient has established risk factors, including:
- Parent with known dyslipidemia
- Family history of early CVD
- Hypertension
- Obesity
- Tobacco use
- Diabetes (type 1 and type 2)
- Kidney disease
- Heart transplant
- Kawasaki disease
- Chronic inflammatory disease
- HIV
- Nephrotic syndrome

Interpreting Lipid Values
Nonfasting and fasting lipid panels are used to measure the amount of LDL, HDL and total cholesterol in the blood. Nonfasting panels are typically used for universal screening because the patient does not have to do any preparation for the test. However, if the nonfasting panel is abnormal or borderline, a fasting lipid panel should be done for more accurate assessment.
Nonfasting: Non-HDL cholesterol should be less than 145, and HDL should be above 40.

How to Treat Dyslipidemia in the Pediatric Patient
The NHLBI guidelines focus on lifestyle modification for the first six months after diagnosis in nearly all patients. Much of the initial management of identified CVD risk factors can be done in the primary care setting if nutrition support and other lifestyle counseling are available. When lifestyle modifications fail to reduce the lipids to the desired level in patients with extreme lipid disorders, pharmacotherapy is recommended.
The back panel of this practice tool provides sample diet and exercise recommendations to help you get started. For more information about diet and exercise in children with borderline-to-high cholesterol, call 877-925-0363 to speak with a specialist.
Family Guide to Diet and Exercise Recommendations
The following recommendations are good for everyone but are of particular importance for people who are at risk for cardiovascular disease. Making healthy choices now is the foundation for a healthy heart into adulthood.
Exercise guidelines: Exercise 60 minutes every day divided among aerobic, bone loading and muscle strengthening physical activities. If you are currently inactive, start with 10 minutes a day or 10 minutes most days and add an additional 5 minutes every week or every two weeks, depending on your ability. It is important to work with your physician on an exercise plan that is accessible and safe.
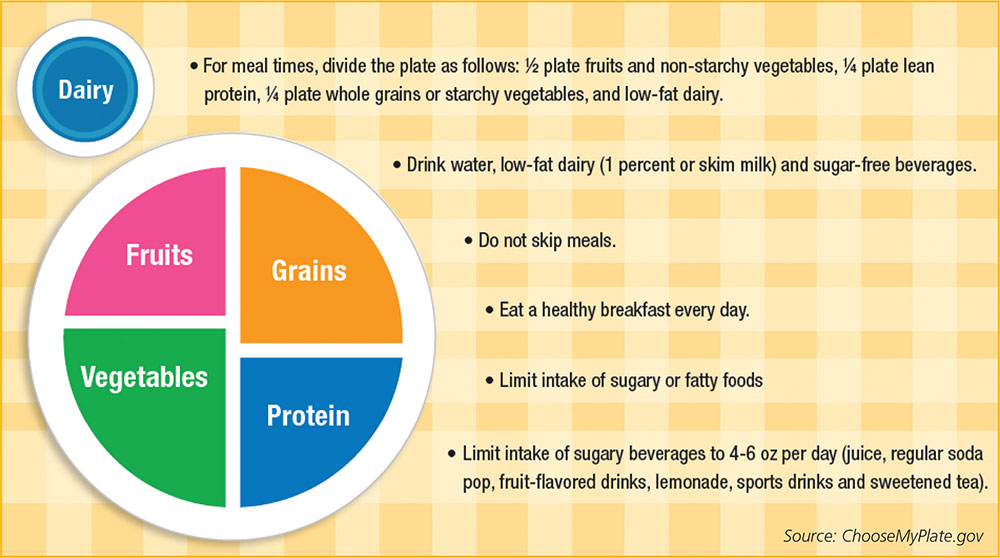
Nutrition guidelines: Follow MyPlate recommendations. More information about MyPlate is available at MyPlate.gov
When to Refer to a Pediatric Cardiologist*
At The Congenital Heart Collaborative, we will see any patient with abnormal fasting lab results. If nonfasting lab results are abnormal, the referring physician should order a fasting lipid panel before the specialist visit.
Urgent referrals are recommended for LDL greater than 190 and triglycerides greater than 500.
* For late adolescent and young adult patients who have no underlying congenital heart disease, you may consider referral to an adult cardiologist.
Contact Us
Physician-to-Physician Consultation Line, 216-UH4-ADOC (216-844-2362)
Physician Access Line, 216-UH4-PEDS (216-844-7337)
(Patient transfers, admissions referrals, emergency department referrals, appointments)