Our History





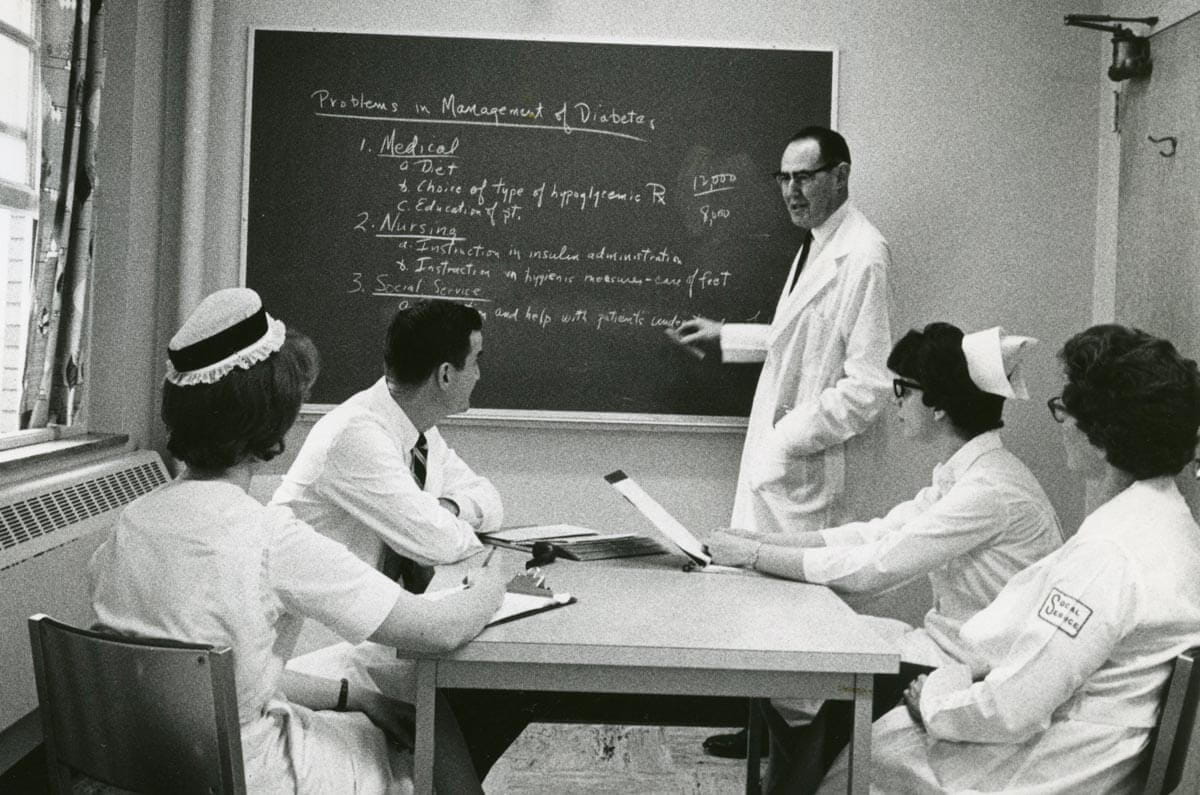
**All photographs courtesy of the Stanley A. Ferguson Archives of University Hospitals of Cleveland.
Major Achievements in Our History
University Hospitals has helped patients living with this condition since the early 1920s, around the same time when insulin became an accepted, effective treatment.
1922: John James MacLeod, MD perfected the use of insulin in diabetic patients and was later awarded a Nobel Prize as a codiscoverer of insulin in 1922. Dr. MacLoeod was on the faculty at the Western Reserve University School of Medicine and began his insulin research there.
1923: Lakeside Hospital received a $10,000 grant from the Rockefeller Institute for Medical Research to assist in covering cost for insulin of patients who could not afford it, along with education of physicians about the new drug and how to administer. The news of the award made front page of the Plain Dealer in 1923.
1960: University Hospitals participated in a nationwide study called the University Group Diabetes Program under Dr. Max Miller’s leadership. This was among the earliest randomized multicenter clinical trials to determine whether lowering blood sugar in diabetic patients would protect against the serious complications of the disease.
Dr. Miller also contributed to studies that were among the first to demonstrate that obesity was a primary risk factor for type 2 diabetes when he observed extremely high insulin levels in many of his obese patients.
Dr. Miller conducted a major research project on the natural history of diabetes among the Pima Indians of Arizona and the effects of diabetes drugs on the overall health of diabetics. He was an internationally known expert on the study and treatment of diabetes. A strong supporter of diet control for diabetes, he was a pioneer in the development of a diet instruction program that involved the patient's family.
Dr. Miller headed a government-sponsored study which found an increased mortality rate from heart disease among diabetics using the oral drug tolbutamide compared to diabetics depending on diet or insulin. He was a consultant to numerous government departments and programs regarding diabetes, metabolic diseases, and retinopathy.
1965: University Hospitals received a grant to fund a project that focused on programmed instruction and education for patients with diabetes that included education about their disease, treatment, and self-management. The award was provided by the U.S. Public Health Service.
1967: Babies & Childrens Hospital began to hold classes for parents of patients with diabetes: teaching how to administer insulin injections, diet management, and best practices for providing their child practical and emotional support.

1970: Biochemist Bernard Landau, MD, Chair of the Endocrinology Division at University Hospitals, furthered the understanding of diabetes and its management through his research. In his studies, he demonstrated “A link between appetite, obesity, and insulin resistance in humans”.
1973: University Hospitals furthered Diabetes research capabilities through a $500,000 gift from Mary Blossom Lee, daughter of former University Hospitals board member Dudley Blossom who had lived with diabetes since early childhood and had supported diabetes research around the country for decades.
In 2000, the University Hospitals Board established the Mary Blossom Lee Chair to advance medical research on the causes, treatment, and consequences of diabetes.
1983: The Diabetes Control and Complications Trial (DCCT), launched by the U.S. National Institute of Diabetes and Digestive and Kidney Diseases, ran from 1983 to 1993. University Hospitals participated in this landmark clinical trial across the United States and Canada that ultimately, for the first time, showed that lowering blood sugar in Type 1 diabetes significantly lowered the risk of developing a number of diabetes-related problems including: vision issues, kidney failure, and nerve damage.
1993: UH endocrinologist Saul Genuth, MD, played a leadership role in the DCCT as a study-wide co-chair and in an extension study called the Epidemiology of Diabetes Interventions and Complications (EDIC), which began in 1993 and is still ongoing today. University Hospitals Rainbow Babies & Children’s Hospitals is the national coordinating center for the project.
2016: University Hospitals pediatric endocrinologist Rose Gubitosi-Klug, MD, PhD, who currently serves as lead investigator of the ongoing study, authored a review of 30 years’ worth of findings the combined DCCT/EDIC studies. The data provided significant insights about type 1 diabetes and the long-term complications associated with it, emphasizing current standards and guidelines for treating patients with the disease.
2020: The UH Diabetes Metabolic Care Center established to provide comprehensive care to patients with diabetes.
2022: A quality improvement research study initiated, utilizing electronic medical records and a diabetes helpline for PCPs to reach out with questions or request recommendations via a chart review, enabling care of over 1,000 patients in the UH system.
2023: University Hospitals was awarded a $2.2 million grant from The Leona M. & Harry B Hemsley Charitable Trust to fund a research project to assist patients classified as emerging adults with Type 1 Diabetes.
2023: University Hospitals received a $1 million grant from the Cleveland Foundation to establish a Midtown Cleveland location to help address obesity, food insecurity, and insulin affordability in vulnerable neighborhoods.


