University Hospitals Partners on $2.78 Million NIH Grant Using AI to Improve Rectal Cancer Treatment
December 16, 2024
Innovations in Digestive Health | Winter 2025
University Hospitals Cleveland Medical Center — in collaboration with Case Western Reserve University, the Cleveland Clinic and Medical College Wisconsin — has secured a five-year, $2.78 million grant from the National Institutes of Health (NIH) and the National Cancer Institute (NCI) to advance the understanding of patient response to rectal cancer treatment. The groundbreaking study is utilizing artificial intelligence-based magnetic resonance imaging (MRI) technology to visualize how rectal tumors respond to therapy.
 Emily Steinhagen, MD
Emily Steinhagen, MD“MRI is the standard-of-care imaging modality for rectal cancer,” says study co-principal investigator Emily Steinhagen, MD, who is leading the clinical integration of the research. Dr. Steinhagen is a colorectal surgeon at University Hospitals Seidman Cancer Center, and the Associate Program Director for the General Surgery Residency Program at University Hospitals. “Through this project, we are harnessing the capabilities of big data and AI to better understand treatment response so that we can predict future patients who would benefit from nonoperative management, which could reduce the need for surgical intervention and enable a significant percentage of individuals to forgo rectal resection.”
According to the American Cancer Society, approximately 46,000 Americans are diagnosed with rectal cancer each year, making it the third-most-common digestive system cancer after colon and pancreatic cancer. Since the mid-1990s, rates of all forms of colorectal cancer have annually been increasing by one to two percent in people younger than 55.
“For a long time, best-practices care for rectal cancer involved chemotherapy, radiation and surgery,” Dr. Steinhagen says. “Now, we can omit surgery in 20 to 30 percent of patients. It is all about selecting them properly.”
Advancing Personalized Treatment
Lead investigator Satish Viswanath, PhD, Associate Professor of Biomedical Engineering at Case Western Reserve University, and his research team are developing radiomic signatures that leverage computational analyses of radiology and pathology images. These advanced AI models will have the capacity to extract specific metrics from MRI scans, offering new insights into disease progression. The findings will address critical challenges clinicians face in assessing which tumors are responding to treatment and which are not.
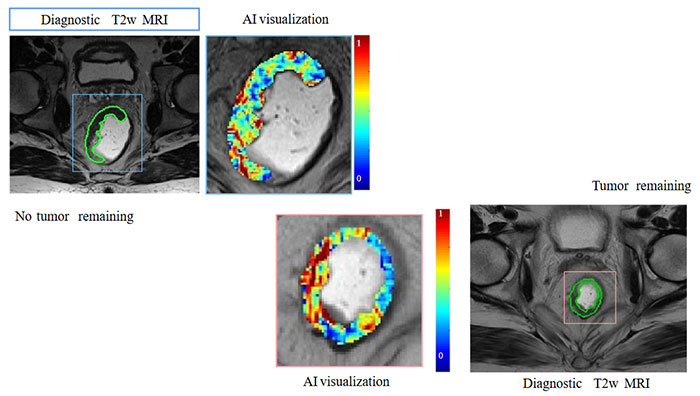
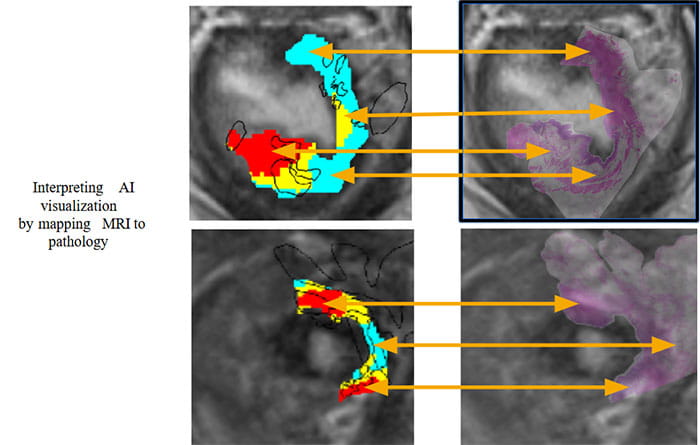
“One of the challenges of monitoring rectal cancer is that we rely on MRI and endoscopy, but to truly prove there are no remaining cancer cells is both difficult and important,” Dr. Steinhagen says. “We are building models that will look for markers of complete clinical response, which we will be able to apply to individual patients in the future to offer them more personalized care and hopefully improve outcomes.”
The study will analyze medical images from over 900 rectal cancer patients, utilizing the novel biology-driven radiomics approach. This includes data collected during previous clinical trials to identify noninvasive and reliable methods of determining which tumors die or significantly regress following therapy. Such advancements could reduce unnecessary surgeries and associated complications. Additionally, researchers hope the project leads to differentiated treatment protocols based on what they learn about patients’ likelihood of having a complete or partial response to current therapy.
“If we know that a patient is unlikely to experience benefit from neoadjuvant treatment, then we could perform surgery sooner,” Dr. Steinhagen says.
Patients with rectal cancer require tremendous amounts of oncological monitoring. “One in five patients with rectal cancer who have a complete clinical response go on to develop a recurrence,” Dr. Steinhagen says. “An exciting aspect of this project is that it could enable us to predict with more certainty who might experience early regrowth and appropriately tailor screening and surveillance protocols.”
Transforming Cancer Care through Collaboration
The project brings together a multidisciplinary team spanning biomedical engineering, radiology, pathology, oncology, biostatistics and surgery. “What I love about the collaborative nature of this project is the opportunity to work with people like Dr. Viswanath, who is the architect of this research, and the experts at the Case Comprehensive Cancer Center,” Dr. Steinhagen says. “The model of team science between these institutions is unparalleled.”
For more information, contact Dr. Steinhagen at Emily.Steinhagen@UHhospitals.org.
Contributing Expert:
Emily Steinhagen, MD
Colorectal Surgeon
Associate Director
General Surgery Residency Program
University Hospitals Cleveland Medical Center
Assistant Professor
Case Western Reserve University School of Medicine


