Executing a Data-Driven Method for Transfusion Management with HemaLogiX™
May 19, 2024
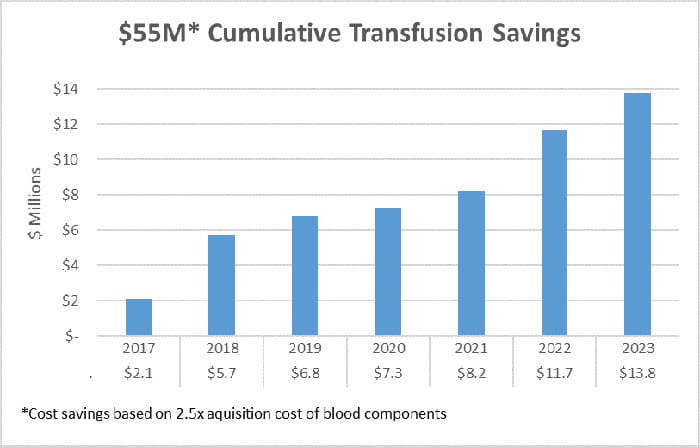
In an era where patient safety and resource management are paramount, University Hospitals In Cleveland, Ohio (UH) saved $55M over 7 years (2017-2023) by pioneering a data-driven and transparent approach for transfusion utilization practices, powered by an innovative analytics platform, HemaLogiX™. The associated costs of transfusion reach well beyond blood acquisition to include handling, processing, supplies to transfuse, and unintentional patient harm.1 While transfusion saves lives, it also carries risk of immediate adverse reactions and unintended complications for patients, and up to 40% of transfusions may not be clinically indicated.2 “Transfusions can save lives, yet blood is scarce, costly, and commonly overused,” shares Dr. Peter Pronovost, Chief Quality and Clinical Transformation Officer at University Hospitals Health System. “The use of a novel technology coupled with a model of transformation reduced our use by decreasing inappropriate transfusions”.
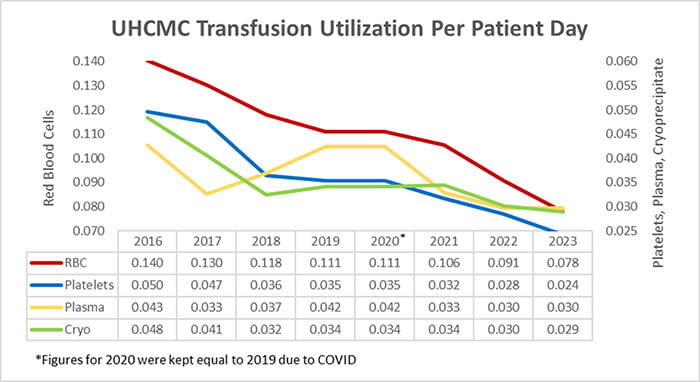
UH began a high reliability medicine (HRM) initiative in 2016 to reduce transfusion overuse and determine how to best measure the prescription of blood for each patient at the time of transfusion. Realizing data is fundamental to identifying opportunity and managing practice change, data was mined and analyzed manually, driving the creation of HemaLogiX and automating the complete analysis of all transfusions in 2017. The automated tool has been crucial to more effectively managing the tenuous blood supply by fine-tuning transfusion practices, resulting in a sustained 45% decrease in red blood cell (RBC) transfusion and 50% decrease in platelet transfusion at UH Cleveland Medical Center. The cumulative financial savings associated with the changes in transfusion of RBC, platelets, plasma and cryoprecipitate exceeded $55M during this time.
“HemaLogiX has been the cornerstone of our strategy, enabling us to take a deep dive into our practices and identify areas with the greatest opportunity for improvement,” says Dr. James Hill, Critical Care Anesthesiologist, Community Hospital COO, HRM Lead, Program Director and Co-inventor of HemaLogiX. “Leveraging the Transfusion Appropriateness Algorithm, which was developed with input from over 30 subspecialists, the platform harnesses clinical data from the EMR and blood management system to provide a rapid, evidence-based assessment of each transfusion.”
The software's sophisticated analytics allow for a granular view of transfusion practices, identifying cases where clinical situations at the time of treatment did not support the prescribed transfusion.3 The ability to aggregate and sort data by facility, department, and provider proved invaluable, offering a clear view of performance, pinpointing where targeted interventions could yield the most significant enhancements. “With HemaLogiX, we could quickly discern patterns and variations across service lines and tailor our educational efforts where they were needed most,” adds Jen Dawson, MBA, MSN, RN, HRM Lead, and Co-inventor of HemaLogiX, who helped leaders and physicians use data to drive performance improvement.
“Moreover, the user-friendly interface of HemaLogiX has facilitated patient chart reviews, allowing caregivers to drill down into specific cases for a thorough analysis. This feature has not only improved understanding of transfusion practices but also fostered an environment of continuous learning and quality improvement,” notes Dr. Daniel Asher, Cardiothoracic Anesthesiologist at UH and CMO of Hemaptics.
Beyond the economic benefits, the true value of HemaLogiX lies in enhancing patient care by ensuring that every transfusion is provided at the most beneficial time to reduce risk to patients. Reductions of overuse further support patient care by ensuring the availability of donated blood to those in need. The successful reductions in use overlap a period of time (2017-2021) when volumes across the United States remained static according to the National Blood Collection and Utilization Survey.4 As a result of the success at UH Cleveland Medical Center, UH has expanded the use of HemaLogiX to its community hospitals.
Looking to the future, UH created a spinoff company, Hemaptics, to expand the capabilities and reach of HemaLogiX. Hemaptics is piloting HemaLogiX at other healthcare systems to quantify the impact on their transfusion utilization. In parallel, Hemaptics has developed a functioning Best Practice Alert (BPA) based on the assessment of each transfusion at the time of ordering. The use of enhanced analytics behind the BPAs is expected to increase attention to the alerts and their influence on prescribing practices. Hemaptics will work with UH and early adopters of HemaLogiX to pilot the BPAs while soliciting feedback for additional enhancements to the application and the methods applying data to drive performance.
Contributing Authors:
James Hill, MD, MBA
Chief Operating Officer, UH Parma Medical Center
Critical Care Anesthesiologist
Assistant Professor
Case Western Reserve University School of Medicine
Daniel Asher, MD
Cardiothoracic Anesthesiology
Department of Anesthesiology and Perioperative Medicine
University Hospitals
Assistant Professor
Case Western Western University School of Medicine
Jen Dawson, MBA, MSN, RN
Sr Operations Engineer
University Hospitals
Craig Schwabl
VP, IT Digital Solutions and Enterprise Analytics
University Hospitals
In addition, support was provided by Dr. Peter Pronovost and many others at UH who contributed input for this work.
Healthcare systems interested in learning more about HemaLogiX for transfusion management should contact the CEO of Hemaptics, Ethan Cohen, at ecohen@hempatics.com.
1 Shander A, Hofmann A, Ozawa S, et al. Activity-based costs of blood transfusions in surgical patients at four hospitals. Transfusion. 2010; 50(4):753-765.
2 Shander A, Fink A, Javidroozi M, et al. Appropriateness of allogeneic red blood cell transfusion: The international consensus conference on transfusion outcomes. Transfus Med Rev. 2011; 25(3):232-246.e53.
3 Dawson J, Schwabl C, Pronovost P, et al. Transfusion utilization and appropriateness: Thinking differently at a tertiary academic medical Center. Physician Leadersh J. 2022; 9(4):18-23.
4 Free R, Sapiano M, Chavez Ortiz J, et al. Continued stabilization of blood collections and transfusions in the United States: Findings from the 2021 National Blood Collection and Utilization Survey. Transfusion. 2023; 63(S4):S8-18.
Tags: Quality Care, Publications


