UH Harrington Heart & Vascular Institute Leads Pivotal Study of LimFlow Therapy for Chronic Limb-Threatening Ischemia
June 22, 2023
Findings published in The New England Journal of Medicine show new therapy saves most patients from amputation
Innovations in Cardiovascular Medicine & Surgery | Summer 2023
New research from University Hospitals Harrington Heart & Vascular Institute shows that there may finally be a viable alternative to amputation for patients suffering from chronic limb-threatening ischemia (CLTI), the most severe form of peripheral artery disease. A study recently published in The New England Journal of Medicine could lead to the first approval by the U.S. Food and Drug Administration of a therapy giving thousands of patients hope for an alternative to limb loss.
 Mehdi Shishehbor, DO, MPH, PhD
Mehdi Shishehbor, DO, MPH, PhDThe PROMISE II U.S. pivotal clinical trial found that minimally invasive LimFlow therapy enabled most patients to avoid amputation and experience wound healing.
UH Harrington Heart & Vascular Institute president Mehdi Shishehbor, DO, MPH, PhD, Angela and James Hambrick Chair in Innovation, is first author of the NEJM paper and co-principal investigator of the multi-center PROMISE II trial.
“Approximately 20 percent of patients with CLTI have no revascularization options, leading to above-ankle amputation,” Dr. Shishehbor says. “Transcatheter arterialization of the deep veins (TADV) is a percutaneous approach that creates an artery-to-vein connection to deliver oxygenated blood via the venous system to the ischemic foot to prevent amputation. LimFlow is a unique and novel alternative to major amputation, providing hope where previously there has been none. The results from this study are excellent and it’s very clear that LimFlow is a powerful tool for avoiding amputation.”
UH is the only site in Ohio to participate in the study.
Study Results
In the paper entitled “Transcatheter Arterialization of the Deep Veins in Chronic Limb-Threatening Ischemia: The PROMISE II Multicenter Prospective Study,” investigators evaluated 105 CLTI patients who were treated with TADV using the LimFlow therapy. All patients were facing inevitable amputation before the procedure. At six months post-procedure, 76 percent of patients were able to keep their leg. Within the same time period, 76 percent of patients had completely healed or healing wounds. Freedom from all-cause mortality was 87 percent at six months.
In the study, the median age of participants was 70 years, with a range of 38 to 89 years old. The study was designed to include diversity, with 31 percent of patients being female and 43 percent being Black, Hispanic, or Latino. The inclusion of a large number of non-white CLTI patients was important because they are disproportionally at risk of amputation compared to white patients.
Behind the Technology
Dr. Shishehbor explains the TADV process: “TADV is an endovascular revascularization procedure for no-option CLTI patients. In TADV for the lower extremities, an arteriovenous fistula is created proximal to the diseased tibial arteries using a covered stent. The oxygenated blood is then diverted from the tibial arteries to the tibial veins to bypass the severely diseased arterial vasculature. The venous system is leveraged to deliver oxygenated arterial blood to the foot through the pedal veins, potentially avoiding major amputation and promoting wound healing.
The PROMISE I study established the feasibility of TADV for the treatment of no-option chronic limb-threatening ischemia, and the PROMISE II trial expanded upon this work to evaluate the effect of TADV on amputation-free survival and limb salvage as compared to an objective performance goal.”
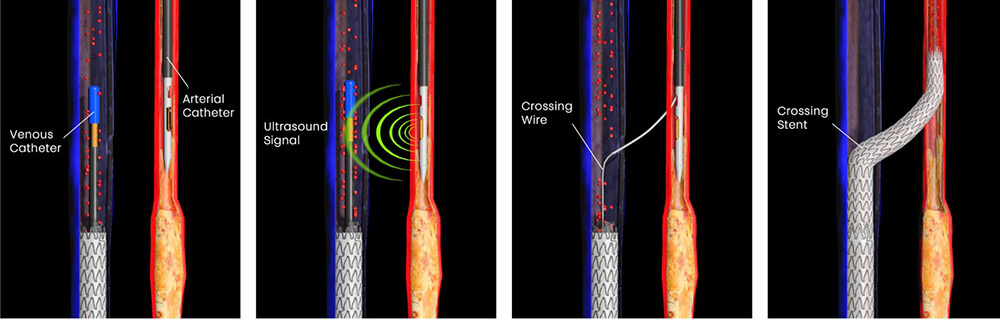 LimFlow procedure.
LimFlow procedure.Alternatives to Amputation
Dr. Shishehbor says it’s hard to overstate the difference this new technology may play in helping CLTI patients avoid amputation. As it stands, it’s an outcome he and his colleagues work assiduously to avoid as much as possible. For example, Dr. Shishehbor leads a Limb Salvage Advisory Council within the UH Harrington Heart & Vascular Institute, unique in the U.S., which engages diverse medical experts from across the UH health system. The panel thoroughly review and discuss each patient slated for amputation – quickly and in real-time. Vascular surgeons, endovascular interventionalists, vascular medicine specialists, podiatrists and wound care experts all participate.
“Every patient deserves at least a second and even a third revascularization attempt using various approaches and sometimes different skill sets to save his or her limb,” Dr. Shishehbor says.
Results published in 2022 show that this innovative approach to quality is working. A study published in Circulation: Cardiovascular Interventions reveals that the LSAC at UH saved the limbs of about 75 percent of the people they worked on – a first in the field.
“We never take amputation lightly,” Dr. Shishehbor says. “While it can alleviate some issues related to disease, it brings its own challenges which can include disability, emotional distress, and even death. Major amputation for CLTI is associated with a 50 percent mortality rate within a year for patients over age 65, and this mortality rate increases in patients with cardiovascular comorbidities.”
With the recent NEJM results of the PROMISE II trial, Dr. Shishehbor says he’s cautiously optimistic that the tide appears to be turning for these patients.
“These patients are literally called ‘no-option’ patients,” Dr. Shishehbor says. “No option means no hope. With this study, we are providing hope for a safe and effective alternative to amputation and a better life for thousands of patients. Once approved by the FDA, we look forward to this procedure being widely available to patients who so desperately need it.”
To refer a patient for consultation with the Limb Salvage and Amputation Prevention Program, call 216-844-3800.
Contributing Expert:
Mehdi Shishehbor, DO, MPH, PhD
President
University Hospitals Harrington Heart & Vascular Institute
Angela and James Hambrick Chair in Innovation
Professor
Case Western Reserve University School of Medicine


