Building and Growing a Multidisciplinary Venous Care Program
February 19, 2023
Innovations in Cardiovascular Medicine & Surgery | Winter 2023
Established in 2021, the Center for Comprehensive Venous Care (CVCC) within University Hospitals Harrington Heart & Vascular Institute has experienced tremendous growth under the direction of Karem Harth, MD, MHS, a vascular surgeon in University Hospitals Harrington Heart & Vascular Institute.
 Karem Harth, MD
Karem Harth, MDYear-over-year, 2022 saw a 77 percent increase in outpatient vein procedures at the center’s primary site in Broadview Heights, Ohio. “We’ve increased the capacity of the center to care for our growing patient volume and have had multiple physicians and trainees come through to learn advanced venous management and techniques,” says Dr. Harth. The CVCC now has a full-time clinical coordinator and is exploring opportunities to expand further into Cleveland’s East- and Westside communities to offer comprehensive, expert treatment across the spectrum of venous conditions.
“We are fortunate to be part of a quaternary health center and utilize the resources of the nationally recognized Harrington Heart & Vascular Institute,” says Dr. Harth. “In treating complex venous conditions, we collaborate with an excellent team of vascular medicine specialists, interventional cardiologists and radiologists.” Additionally, Dr. Harth leads a monthly multidisciplinary venous conference to discuss complex patient cases that arise throughout University Hospitals Health System.
The center’s offerings include:
- Advanced diagnostic imaging capabilities
- Minimally invasive therapies, including embolization, endovenous ablation and sclerotherapy
- Pelvic venous disease evaluation and treatment via minimally invasive and open surgical options
- Endovenous therapies for acute and chronic deep vein thrombosis (DVT)
- Endovenous options for challenging occlusions of inferior vena cava (IVC) or iliac veins
- Complex IVC filter retrieval
Retrospective Clinical Studies in Pelvic Venous Disease
In addition to offering state-of-the-art clinical therapies, the team is advancing care equity in venous research, focusing on women’s health and pelvic venous disease. “We’re initiating multiple clinical retrospective studies to understand how we can better identify patients who would benefit from available therapies,” says Dr. Harth.
Pelvic congestion syndrome (PCS) is a chronic condition that can cause unrelenting pain. “Our experience is that too many of these patients are not receiving appropriate insurance coverage, diagnosis, referral or treatment,” says Dr. Harth. “A better understanding of current patient management pathways for PCS will provide opportunities to promote increased awareness of low-risk therapies that have the potential to bring relief to women who too often feel they have nowhere to turn.”
Anecdotal evidence suggests a gender bias in coverage for coil embolization procedures to address pelvic congestion. “We are looking at healthcare coverage patterns for therapies that address pelvic congestion in women,” explains Dr. Harth. “There is considerable inequity in coverage for procedures that provide excellent outcomes in properly selected patients, so we hope to shed some light on the data in a scientific manner.”
Researchers are starting with Ohio’s health insurance landscape and will expand to understanding limitations of coverage on a national level.
“Pelvic congestion in women is poorly understood and often goes underdiagnosed and therefore undertreated, but effective treatments are available,” says Dr. Harth. “We know that appropriately selected patients respond well to these minimally invasive procedures, but much work needs to be done to ensure equity in care access and affordability.”
Clinical Multicenter Novel Bioprosthetic Valve Trial
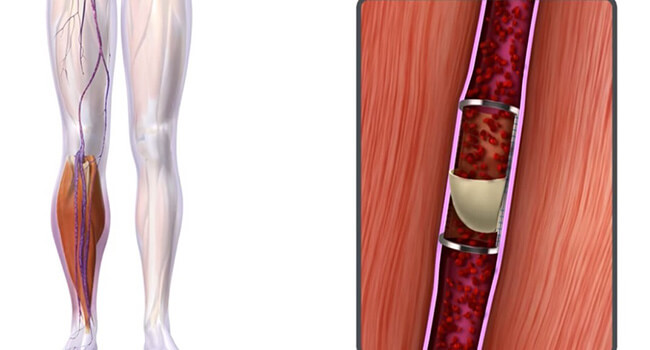 Surgical Anti-reflux Venous Valve Endoprosthesis (SAVVE) Ongoing Pivotal Study to Evaluate VenoValve® for the Treatment of Chronic Venous Insufficiency.
Surgical Anti-reflux Venous Valve Endoprosthesis (SAVVE) Ongoing Pivotal Study to Evaluate VenoValve® for the Treatment of Chronic Venous Insufficiency.The CVVC is one of 22 sites around the country selected to participate in the SAVVE trial, a multicenter investigation of the safety and efficacy of Hancock Jaffe Laboratories’ VenoValve®, a first-in-class bioprosthetic for the treatment of severe, deep chronic venous insufficiency (CVI). The study targets patients with deep venous reflux who have advanced venous disease and symptoms such as debilitating leg pain, swelling or ulceration.
“We have very good long-standing therapies for superficial venous disease in the legs but lack options for treatment of deep venous disease. This trial is exciting because early data on the surgically implantable prosthetic valve has been encouraging for wound healing and symptom control,” says Dr. Harth. “We are very fortunate to be able to offer this novel therapy to our community.”
For more information or to learn about study eligibility, please contact Dr. Harth at 216-844-3013 or Karem.Harth@UHhospitals.org.
Contributing Expert:
Karem Harth, MD, MHS
Director, Center for Comprehensive Venous Care
University Hospitals Harrington Heart & Vascular Institute
Associate Professor of Medicine
Case Western Reserve University School of Medicine


