University Hospitals Harrington Heart & Vascular Institute Tests Pioneering Aortic Arch Stent Graft
November 14, 2022
Innovations in Cardiovascular Medicine & Surgery | Fall 2022
University Hospitals Harrington Heart & Vascular Institute is the only program in Northeast Ohio, and one of two in the state, testing the pioneering Nexus® aortic arch stent graft system to treat thoracic aortic lesions involving the aortic arch.
 Jae S. Cho, MD
Jae S. Cho, MD Yakov Elgudin, MD, PhD
Yakov Elgudin, MD, PhD“This is the first off-the-shelf stent graft developed to provide total endovascular aortic arch repair,” says Jae S. Cho, MD, Co-Director of the Aortic Disease Center within University Hospitals Harrington Heart & Vascular Institute. “The system’s minimally invasive approach and innovative design are advancing treatment of complex thoracic aortic arch pathology and significantly minimizing the risks associated with traditional open surgery.”
Dr. Cho and Yakov Elgudin, MD, PhD, Senior Attending Cardiac Surgeon within University Hospitals Harrington Heart & Vascular Institute, are Co-Principal Investigators for the TRIOMPHE trial, a Food and Drug Administration (FDA)-approved investigational device exemption (IDE) study. Drs. Cho and Elgudin have successfully placed their first two Nexus stent grafts as part of this trial.
They are among a select group of cardiac and vascular surgeons evaluating the safety and efficacy of the branched aortic arch device, manufactured by the Israeli-based company Endospan. “Our first patient was 65, and the second was 75,” Dr. Cho says. “Both experienced optimal outcomes in short-term follow-up.” Approximately 30 centers throughout the United States and New Zealand are participating in the pivotal multi-arm, non-randomized trial, which aims to enroll a total of 100 patients. In the coming year, the team will continue to enroll patients at University Hospitals who are 18 years or older and meet the trial’s inclusion criteria.
Open Vs. Endovascular Aortic Arch Repair
While endovascular techniques have become standard care for abdominal aortic aneurysms, patients with pathology involving or extending into the aortic arch — including chronic dissections, aneurysms, penetrating aortic ulcers and intramural hematomas — have had limited treatment options. Until now, Dr. Cho explains, these repairs would have required two extensive open-chest surgeries.
“Many patients with thoracoabdominal aneurysm are too medically fragile for complex surgeries,” he says. “Advanced age or comorbidities exclude them as candidates for open repair.” Now, they may have another choice. “If successful, the use of Nexus endograft will open up a new era in the management of a very complex aortic arch disease, including aortic arch aneurysms and dissections,” adds Dr. Elgudin.
 Nexus® aortic arch stent graft system.
Nexus® aortic arch stent graft system.
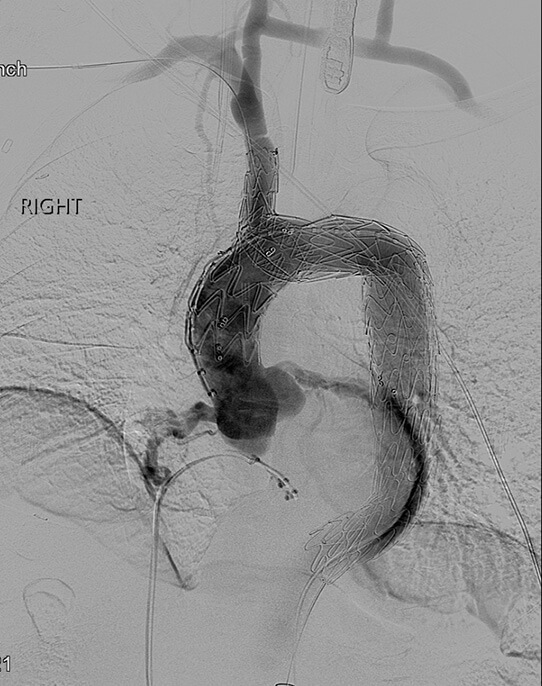 Aortic arch stent device in place.
Aortic arch stent device in place.
- Open repair - Stage one of the complex open procedure involves opening the chest through the sternum, reconstructing the ascending aorta and bypass-grafting the carotid and subclavian arteries. Stage two occurs about six weeks later, after the patient is allowed to recover from the first operation. A second open surgery requires a long incision through the thoracic and abdominal cavities for primary repair of the aneurysm. The procedure is invasive and may be associated with various complications; patients face several weeks of recovery.
- Endovascular repair with Nexus aortic arch stent graft system - In stage one, the surgeon uses open techniques through a small incision in the neck to reroute cerebral and upper extremity blood flow by bypassing from the right carotid artery to the left carotid artery and the left subclavian artery. This technique avoids the need for open-chest surgery. Two to three days later, incisions in the groin enable deployment of the stent graft into the aortic arch and into the ascending aorta with a side branch graft into the innominate artery. Patients are typically able to return home a couple of days later.
The Future of Total Endovascular Arch Repair
The Nexus stent graft configurations are engineered to accommodate a range of anatomies and can be adjusted for the length and diameter of the ascending innominate artery and descending aorta. Stable anchoring of the deployed stent graft provides a durable and lasting repair, while the minimally invasive procedure reduces risk of postoperative complications. Additional benefits include procedural consistency, efficient healthcare resource utilization, reduced risk of infection and improved patient comfort.
“Our participation in the TRIOMPHE trial showcases our dedication to optimizing treatment options for our complex aortic patients,” says Dr. Cho. “We continue to lead the way as providers of novel endovascular medicine for our Northeast Ohio communities and beyond.”
For more information, contact Dr. Cho at Jae.Cho@UHhospitals.org or Dr. Elgudin at Yakov.Elgudin@UHhospitals.org.
Contributing Experts:
Jae S. Cho, MD
Co-Director, Aortic Disease Center, and Co-Director, Vascular Center
Brenda and Marshall Brown Master Clinician in Vascular Innovation
University Hospitals Harrington Heart & Vascular Institute
Professor
Case Western Reserve University School of Medicine
Yakov Elgudin, MD, PhD
Senior Attending Cardiac Surgeon
University Hospitals Harrington Heart & Vascular Institute
Associate Professor
Case Western Reserve University School of Medicine


