University Hospitals Harrington Heart & Vascular Institute OFFERS HAART™ Aortic Valve Repair Technology
February 03, 2022
Innovations in Cardiovascular Medicine & Surgery | Winter 2022
While mitral valve repair has advanced over the past decade, those innovations have not translated to the aortic space until recently. “We’re seeing a movement in cardiac surgery to explore aortic repair,” says Gregory Rushing, MD, a cardiac surgeon at University Hospitals Harrington Heart & Vascular Institute.
 Gregory Rushing, MD
Gregory Rushing, MDThe geometry of both valves is complex, but a limiting factor has been that the incidence of mitral valve regurgitation far exceeds aortic regurgitation. Approximately a third of aortic insufficiency is driven by aneurysms, typically affecting a younger population.
“Aortic replacement is a fantastic technology, but a bioprosthesis has a lifespan of only 10 to 12 years,” Dr. Rushing says. “The question has been, ‘What can be done to limit exposure to multiple operations and provide these patients with a durable repair?’”
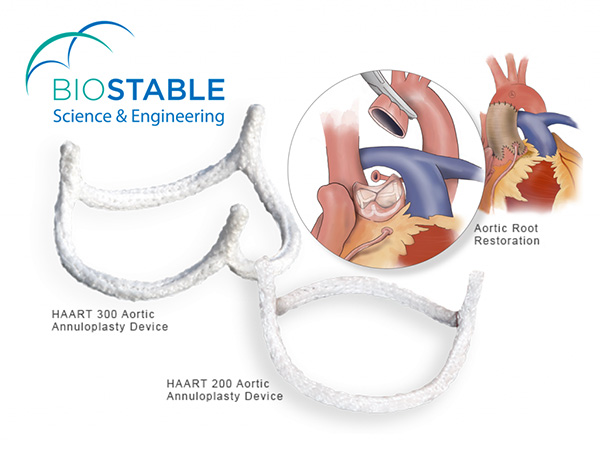
Along with colleagues Alan Markowitz, MD, Cardiac Surgical Director, UH Harrington Heart & Vascular Institute at UH Ahuja Medical Center, the Marcella "Dolly" Haugh Chair in Valvular Surgery, University Hospitals; and Clinical Assistant Professor of Surgery at Case Western Reserve University School of Medicine and Pablo Ruda Vega, MD, Cardiac Surgery, UH Harrington Heart & Vascular Institute; and Clinical Associate Professor at the School of Medicine. Dr. Rushing is now treating aortic insufficiency utilizing HAART™ aortic valve repair technology. Developed by BioStable Science & Engineering Inc., the procedure is the first reproducible means of creating normal three-dimensional aortic annulus architecture.
University Hospitals Harrington Heart & Vascular Institute is the only approved site in Northeast Ohio and one of three in the state offering the advanced surgical procedure.
The HAART device, composed of Dacron-skirted titanium, is an elliptical annuloplasty ring based on high-resolution CT angiograms of healthy aortic valves. Available for both tricuspid and bicuspid anatomy, it is implanted below the leaflet aortic junction to stabilize the valve and serve as a framework for improved coaptation.
“There are maneuvers, such as commissure resuspension or leaflet plication, you can utilize to repair the leaflets,” Dr. Rushing says. “However, if you don’t do something to support the valve structure, too much tension causes the repair to fail.”
Successful aortic repairs
The three cardiac surgeons performed their first cases early this year. “To become an FDA-approved site, we had a fairly intensive hands-on proctoring process,” Dr. Rushing says. “After extensive education, we scheduled the first two patients for a Monday and Tuesday and set up a wet lab the preceding weekend to get a feel for the technique.”
So far, the team has placed five devices with excellent outcomes. Three of the five patients have passed the six-month mark, and echocardiograms show no residual aortic regurgitation.
In one particularly complex case, a woman has since had additional surgeries. “The patient had aortic insufficiency, but she also had ascending, arch and descending aortic aneurysms,” Dr. Rushing says. “We replaced her ascending aorta and the arch of the aorta in conjunction with the ring repair. Next she had a subsequent endovascular aneurysm repair of the descending thoracic aorta. Then, about a month ago, she had a thoracoabdominal aneurysm repair, so her whole aorta has been replaced over the last six months.” With each additional procedure, her aortic valve repair held.
Patient selection and tracking
For a valve to be amenable to repair, it must be free from stenosis, endocarditis or significant leaflet destruction. Because the appropriate patient parameters are narrow, each member of the team has scrubbed in for all five procedures to gain experience and reduce lag time between cases. Currently, they are screening several additional patients to determine if aortic repair is a viable solution.
A multi-center clinical trial of the HAART 300 (tricuspid) device is demonstrating favorable evidence of safety and efficacy, including low morbidity and no in-hospital mortality and a 95 percent survival rate at the mean two-year follow-up. “We’re excited to add this tool to our tool belt,” Dr. Rushing says. “By repairing the native anatomy, we’re correcting valve insufficiency without the risks associated with prosthesis-related complications, thrombosis or oral anticoagulation.”
To learn more or refer a patient, call 216-844-4004.
Contributing Expert:
Gregory Rushing, MD
Cardiac Surgery Director
University Hospitals Parma Medical Center
University Hospitals Harrington Heart & Vascular Institute
Associate Professor
Case Western Reserve University School of Medicine


