University Hospitals Harrington Heart & Vascular Institute First in U.S. to Report New Minimally Invasive Approach to Treat Infective Endocarditis
November 10, 2021
New strategy could revolutionize care for difficult-to-treat patients
Innovations in Cardiovascular Medicine & Surgery | Fall 2021
A team of interventional cardiologists and cardiac surgeons at University Hospitals Harrington Heart & Vascular Institute are the first in the U.S. to report a safer, minimally invasive strategy for removing vegetations in the heart associated with right-sided infective endocarditis – common among IV drug users, people on dialysis and people with indwelling catheters. The procedure, using the FlowTriever system with FLEX technology originally designed to treat pulmonary embolism, is conducted in the catheterization lab on an awake patient – no operating room, intubation or heart-lung bypass machine required. The novel procedure employs intracardiac echocardiography and fluoroscopy guidance, eliminating the need for uncomfortable transesophageal echocardiography for the patient.
Mehdi H. Shishehbor, DO, MPH, PhD, President of University Hospitals Harrington Heart & Vascular Institute and the Angela and James Hambrick Master Clinician in Innovation, reported the first case in the journal Catheterization & Cardiovascular Interventions. Since then, he and his team have completed an additional 13 successful cases.
 Mehdi Shishehbor, DO, MPH, PhD
Mehdi Shishehbor, DO, MPH, PhD Yasir Abu-Omar, MD
Yasir Abu-Omar, MDInfective endocarditis has traditionally been very challenging to treat with two less-than-ideal surgical and interventional cardiology options, Dr. Shishehbor says.
“Many of these patients would typically require open-heart surgery,” he says. “We also have the AngioVac system, but it is not very patient-friendly. It’s a stiff, straight catheter and not something you can bend or move around. Because of that, it’s not ideal for maneuvering within the heart. It’s also much more complicated. It requires the patient to be in the OR, under general anesthesia and requires a heart-lung machine to do the procedure. So it’s a much bigger, much more intense, much more costly procedure.”
The new Triever option does not have these disadvantages, Dr. Shishehbor says.
“The beauty of the new technology is that it can be done on an awake patient, does not require a heart-lung machine, does not require general anesthesia, and the procedure takes about 20 minutes,” he says. “I was optimistic that given my experience with AngioVac, we’d be able to use this new Triever technology in a much safer, less intensive way, to be able to get the vegetations out. We tried it in a patient who was not a good surgical candidate, and we were surprised at how effective it was.”
“This innovative procedure has many advantages for these, often, very sick patients,” adds cardiac surgeon, Yasir Abu-Omar, MD, Director of Cardiothoracic Transplantation and Mechanical Circulatory Support at University Hospitals Harrington Heart & Vascular Institute. “It allows removal of the infected vegetations on the heart valve without the need for an open heart procedure. By removing these, the risk of embolism is minimized and this allows the patient to recover with antibiotic therapy to eliminate the infection. If the need arises, having had this percutaneous procedure with the Triever system does not preclude later surgery. Importantly, this novel strategy demonstrates the very close integration and multidisciplinary relationship between the different specialties in University Hospitals Harrington Heart & Vascular Institute. This is the core for providing the best care for our patients.”
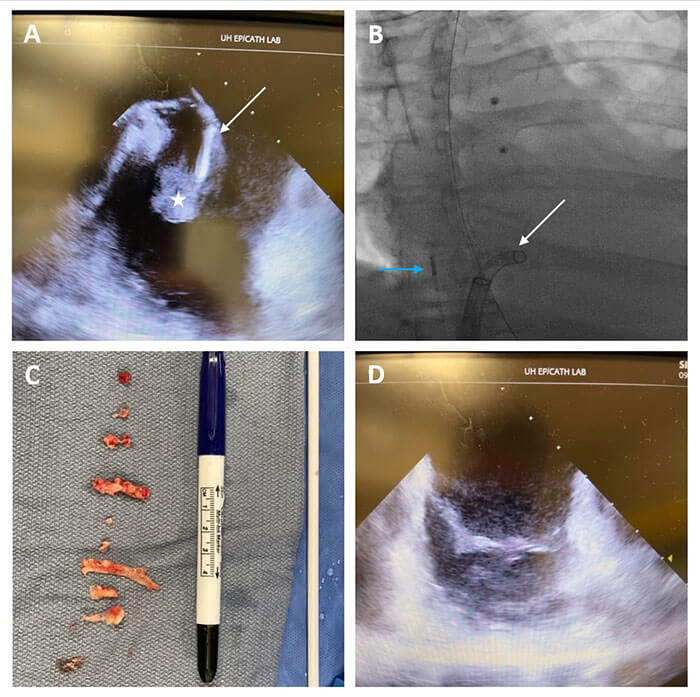 Panels A and B show ICE (blue arrow)-guided percutaneous removal of a large tricuspid valve vegetation (white star) using the Triever aspiration system (white arrow). Vegetation was removed outside the body (Panel C) and repeat ICE confirmed minimal residual valve vegetation (Panel D).
Panels A and B show ICE (blue arrow)-guided percutaneous removal of a large tricuspid valve vegetation (white star) using the Triever aspiration system (white arrow). Vegetation was removed outside the body (Panel C) and repeat ICE confirmed minimal residual valve vegetation (Panel D).Dr. Shishehbor and his colleagues have launched a multi-site registry to further evaluate the potential of the new minimally invasive intervention. However, he says, it could represent a paradigm shift in treating right-sided infective endocarditis, especially among IV drug users. These patients often have their vegetations cleared via surgery or interventional cardiology procedure, only to have them recur due to relapsed IV drug use – making them poor candidates for a second operation.
“This is a true revolution in treating these patients,” Dr. Shishehbor says. “We no longer have to go directly to surgery – we can try this approach first, get the infection out, get the patients discharged from the hospital and get them into substance abuse therapy. If they’ve doing well, then no further surgery is needed, however, if we confirm they need an operation we can offer that after proper rehabilitation. It’s a true paradigm shift.”
Having a minimally invasive first option for these patients is critical, Dr. Shishehbor says, since many are not ideal surgical candidates.
“Most of these patients are deconditioned because of their IV drug use and prolong hospitalization,” he says. “They’re not ideal patients for the OR. It’s early, and we need more data, but in our hospital here at University Hospitals, it has changed clinical practice for all of these patients. As we provide more data, we expect that hospitals will be making this change across the United States.”
For more information on the new minimally invasive approach to infective endocarditis pioneered at University Hospitals Harrington Heart & Vascular Institute, please email HVInnovations@UHhospitals.org.
Contributing Experts:
Mehdi H. Shishehbor, DO, MPH, PhD
President, University Hospitals Harrington Heart & Vascular Institute
Angela and James Hambrick Master Clinician in Innovation
University Hospitals
Professor of Medicine
Case Western Reserve University School of Medicine
Yasir Abu-Omar, MD
Director of Cardiothoracic Transplantation and Mechanical Circulatory Support
University Hospitals Harrington Heart & Vascular Institute
Clinical Professor of Surgery
Case Western Reserve University School of Medicine


