UH Contributes to Valuable Research for Patients with Carotid Artery Disease
January 20, 2020
Studies find TCAR associated with lower risk of stroke and cranial nerve injury
University Hospitals (UH) participates in research that advances the science of health, including several studies published over the past 6 months revealing important information about Transcarotid Artery Revascularization (TCAR).
The body has two carotid arteries – one on each side of the neck. They supply oxygen-rich blood to your brain, head and neck. Carotid artery disease happens when plaques build up in those arteries. It’s a major cause of stroke in the United States.
For decades, surgeons performed carotid endarterectomy (CEA) as the main treatment for this disease. This entails a surgeon making a cut in the neck and removing the blockage. Patients must stay in the hospital for up to three days, including time in the intensive care unit. The procedure is invasive, leaves a scar and can lead to complications.
Transfemoral carotid artery stenting (TFCAS) is a less-invasive alternative where the blockage is reached through a catheter inserted into the leg. But this procedure carries an increased risk of stroke.
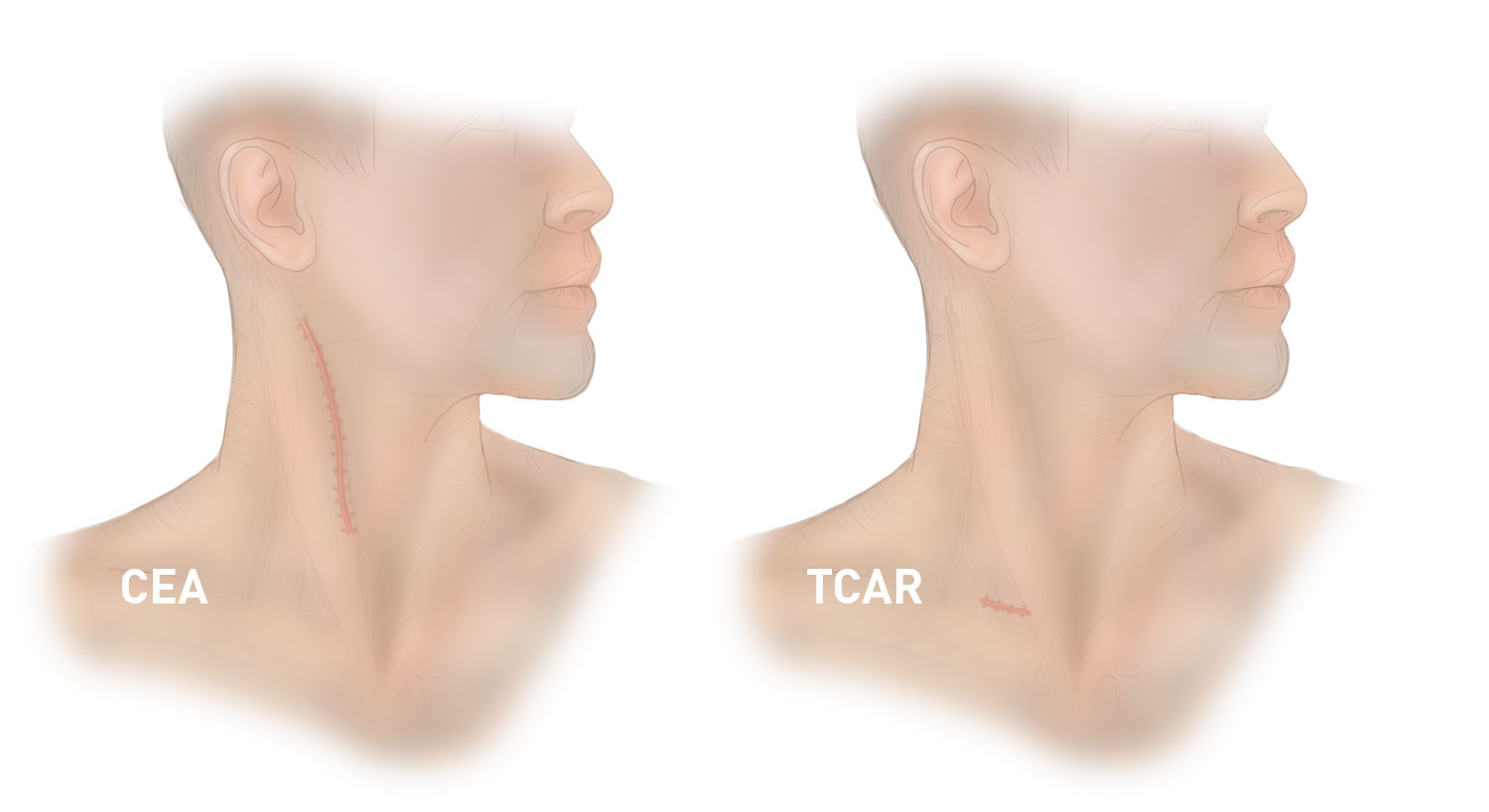 CEA vs. TCAR scar. Photo permission from Silk Road Medical.
CEA vs. TCAR scar. Photo permission from Silk Road Medical.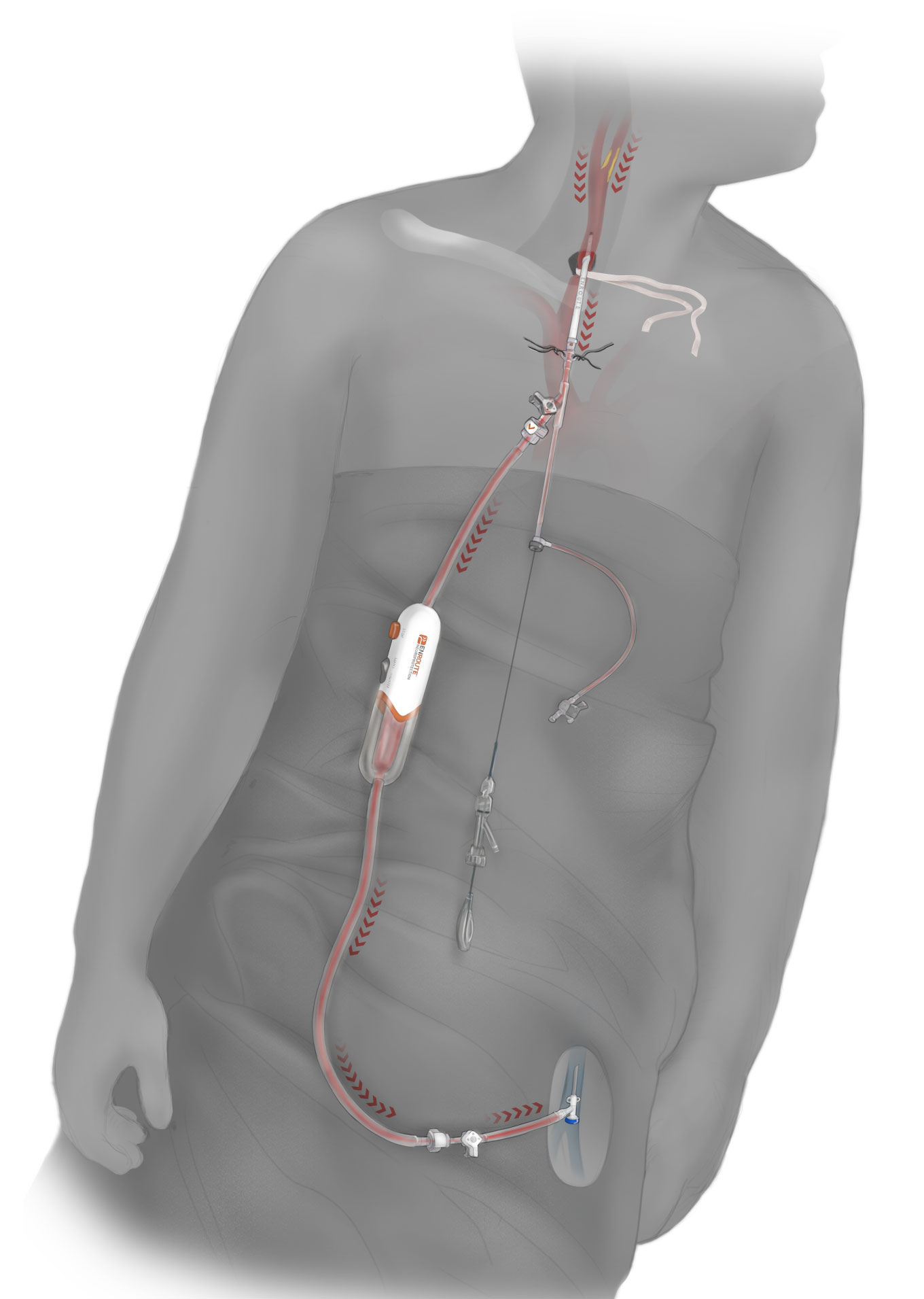 TCAR illustration. Photo permission from Silk Road Medical.
TCAR illustration. Photo permission from Silk Road Medical.Vikram Kashyap, MD, Division Chief, Vascular Surgery at UH has performed TCAR since it was approved by the FDA in 2015. He routinely participates in important research regarding TCAR. Since July of 2019, three respected journals have published papers reporting important findings about the procedure.
Learning Curve for Surgeons Adopting Transcarotid Artery Revascularization Based on the Vascular Quality Initiative-Transcarotid Artery Revascularization Surveillance Project. Journal of the American College of Surgeons (January 2020).
How much experience does it take a surgeon to become an expert in a particular procedure? It turns out, with TCAR, only about 10 times. This paper used data from the Vascular Quality Initiative TCAR Surveillance Project (TSP), a database with information about outcomes of thousands of TCAR cases. The authors, including Dr. Kashyap, analyzed more than 3,000 patients to determine how long it takes a surgeon to become a TCAR expert. They came to the conclusion there is no difference in major in-hospital outcomes for patients, including stroke, death and stroke/death/heart attack together, regardless of the physician’s experience with the procedure.
“In this study, we found physicians can adopt TCAR very safely. The learning curve for this novel procedure is short,” said Dr. Kashyap.
The authors concluded that even in the early stages of learning, surgeons are performing TCAR with excellent stroke and mortality rates.
Association of Transcarotid Artery Revascularization vs Transfemoral Carotid Artery Stenting With Stroke or Death Among Patients With Carotid Artery Stenosis. The Journal of the American Medical Association (December 2019).
This study set out to determine whether TCAR or TFCAS is associated with a lower risk of stroke or death among patients undergoing treatment for carotid artery stenosis.
It analyzed data from thousands of procedures using the TSP and found TCAR was associated with a lower risk of stroke or death compared to TFCAS.
“Performing a prospective randomized trial takes years,” said Dr. Kashyap. “Using the TSP, a registry of thousands of patients, allowed us to answer an important question: In patients with severe carotid disease and high risk co-morbidities, should we use TCAR or TFCAS? The answer is clear. If the patient’s anatomy and other clinical factors allow, TCAR is better.”
A Multi-institutional Analysis of Transcarotid Artery Revascularization Compared to Carotid Endarterectomy. Journal of Vascular Surgery (July 2019).
This study used patient data from a 4-year period to compare TCAR and CEA outcomes at one month and one year post-procedure. It found that patients undergoing TCAR ended up with similar outcomes as those who underwent CEA, with TCAR having a much lower risk of cranial nerve injury.
“In this study, we are comparing TCAR to the gold standard, CEA. This type of clinical research sets the foundation for larger clinical studies that physicians at UH can participate in and lead,” said Dr. Kashyap. “As we learn about novel procedures, we also bring the latest, cutting-edge therapies to our patients in Ohio.”
For more information contact UH Media Carly Belsterling or UH TV Studio at 216-844-2555 or Cell 412-889-8866.
Tags: Stroke, Vascular Disease, Research


