Advances in Rotator Cuff Tendon Repair
May 13, 2019
Innovative patch uses body's natural resources to repair damaged tendons
Innovations in Orthopaedics | Summer 2019
Rotator cuff tendons come into use when we play tennis, throw a baseball or comb our hair. They can tear during a fall or when lifting a heavy object overhead, or they can deteriorate progressively over time. Athletes, workers with jobs that require repetitive lifting, and people over age 50 have a higher injury risk.
Unfortunately, tears that are severe or persistent enough to require rotator cuff surgery may not heal after a procedure. Healing rates vary anywhere from 6 to 90 percent. Age, tear size, fatty infiltration and atrophy all contribute to degeneration and slow healing rates.
According to Ozan Akkus, PhD, Leonard Case Jr. Professor of Engineering, Case Western Reserve University, who established Case Western Reserve University's Orthopaedic Bioengineering Laboratory (OBL), shoulder surgeons face a dilemma: If rotator cuff tissue has degraded too much, there's too much tension when they attempt to reattach the tendon to the bone. “I need to have new material to bridge that gap,” he says.
Akkus and his team have been developing a tendon-like material to do just that for the past 11 years. The results from his latest study indicate he may have succeeded.
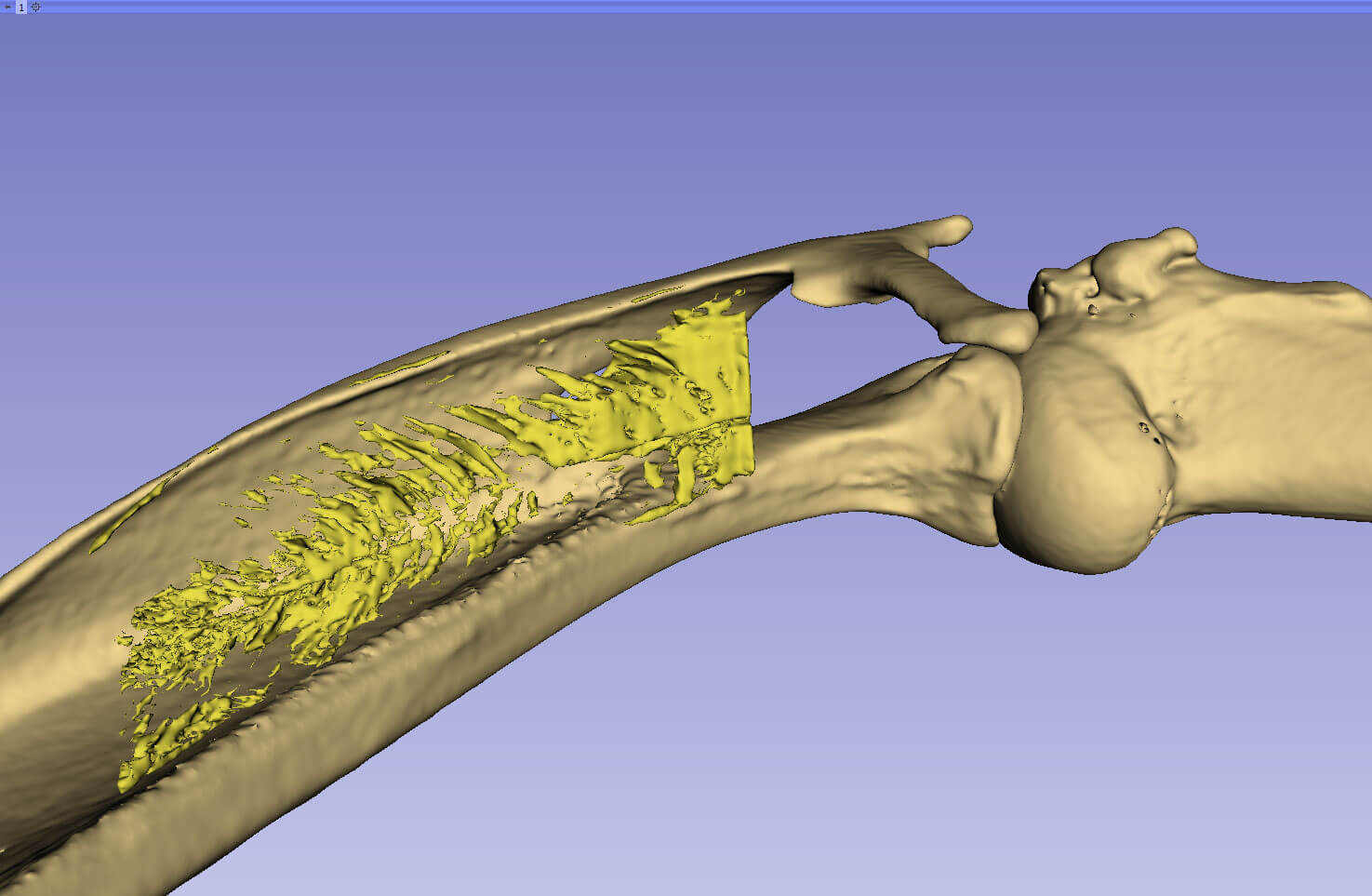
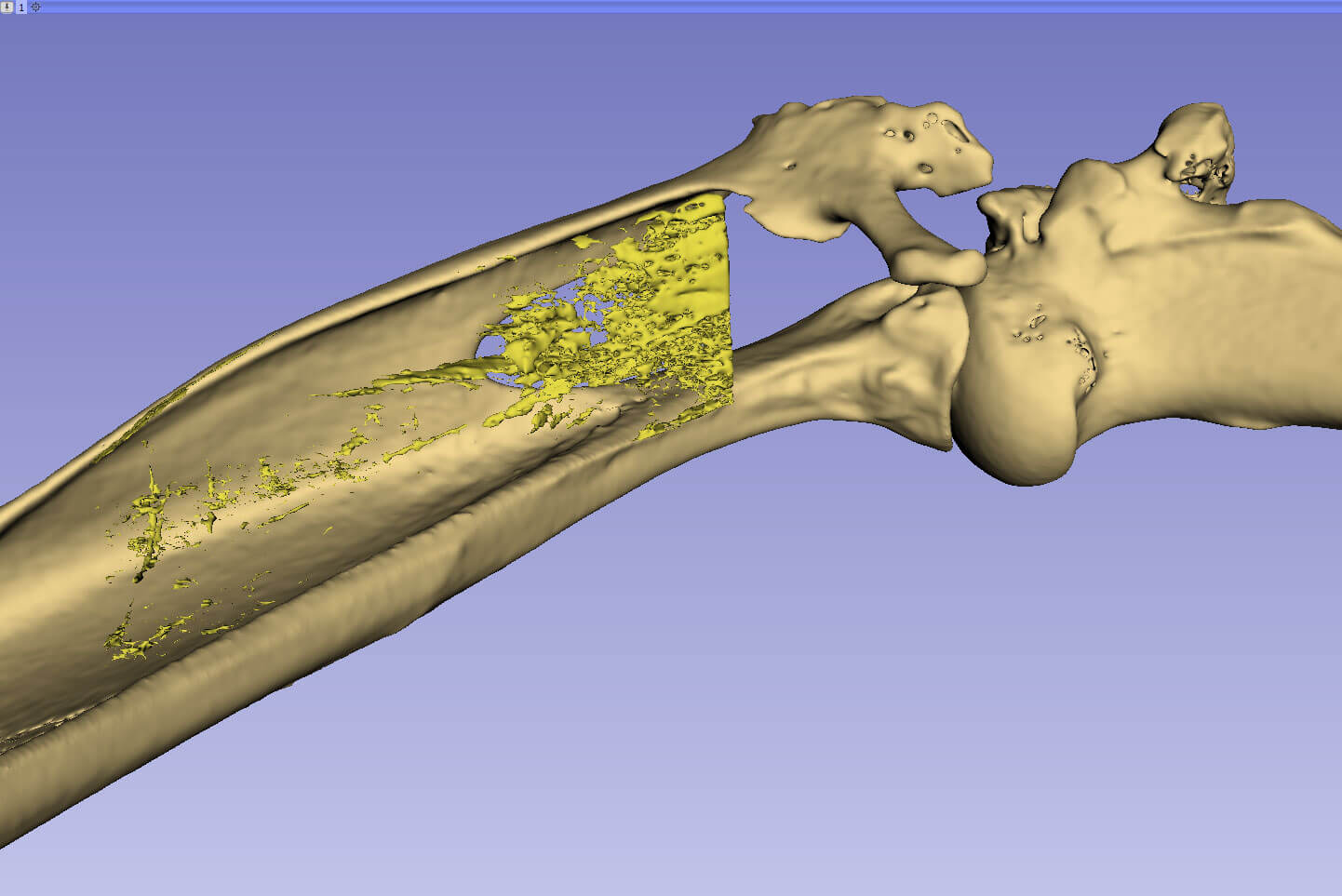
He has developed a scaffold using woven, electrochemically aligned collagen (ELAC) threads. The addition of mesenchymal stem cells (MSC) serves as a supplement to increase stiffness and to regenerate new tissue.
“Our hope is to have a higher success rate in difficult tendon surgeries, as well as increase healing rate and time to return to work,” says Robert Gillespie, MD, Chief of the Shoulder and Elbow Surgery Division of University Hospitals Cleveland Medical Center and University Hospitals Ahuja Medical Center, and Associate Professor of Orthopaedics, Case Western Reserve School of Medicine, “The ELAC scaffold has the potential to be a real game-changer for orthopaedics and rotator cuff surgery.”
HOW IT WORKS
Tendons and other connective tissue are composed primarily of collagen, the ELAC scaffold's key ingredient. When you reconstitute collagen in a lab, you get “something like Jell-O,” Akkus says. To make it stronger, he developed a way to align these stick-like molecules in parallel and in high density. Electric currents pack the collagen into the strong threads that form the scaffold. Stem cells from a patient's bone marrow, obtained via a minimally invasive process, provide the scaffold's regenerative benefits.

“Because this material is so ubiquitous, we can use this technology for blood vessel, cartilage repair… any structural entity in the body,” Akkus says. “We can repair what's currently irreparable.”
ANIMAL STUDIES PROVIDE ENCOURAGING RESULTS
The recent in vivo pilot investigation compared outcomes in rabbits using the ELAC scaffold only, the scaffold plus MSCs, or direct repair. Results showed repairs are comparably stiff and strong between the scaffold and direct repair, but the addition of MSCs made the area even stiffer and stronger. The scaffold with MSCs may also halt fatty infiltration of the attached muscles.
“This is exciting news for rotator cuff repairs,” Dr. Gillespie says. “For people under age 60, we have very few good options. We have shoulder replacement surgery, grafts and tendon transfers. This novel approach to large rotator cuff tears has the ability to last longer and allow return to normal activity without changing the patient’s normal anatomy or the risk of infection seen with total joint replacements.”
Dr. Gillespie says he got involved with Akkus and this project about six years ago because of the scaffold's potential to better heal otherwise irreparable rotator cuff tears. “Ozan is helping create a solution to a problem we don't have a good answer for right now,” Dr. Gillespie says. “I am honored to be able to work with him on this.”
With the pilot study complete, Akkus and team will move to larger animal models, followed by an investigational device exemption (IDE) from the Food and Drug Administration. From there, the team will research the scaffold's compatibility in humans.
Very few new devices, drugs or procedures earn the term disruptive. This could be one of them. “Ozan has spent years developing this,” Dr. Gillespie says. “Very few pieces of technology have the chance to be disruptive in orthopaedic surgery and change the way we treat certain conditions, but this novel graft may have the ability to do that for severe tendon injuries.”
Dr. Robert Gillespie can be contacted at 216-844-7200 , Dr.Ozan Akkus at 216-368-4175.


