Using Radiomics to Improve Crohn's Disease Treatment
November 06, 2018
How science and technology are helping clinicians predict treatment for Crohn’s patients
UH Innovations in Digestive Health - Fall 2018
 Maneesh Dave, MD, MPH
Maneesh Dave, MD, MPH Satish Viswanath, MD
Satish Viswanath, MDAbout 1 million Americans live with Crohn's disease, a chronic inflammatory bowel disease (IBD) marked by inflammation of the digestive tract. Although symptoms vary, they can get worse over time. Complications include fissures, abscesses, fistulas, vitamin and mineral deficiencies, and an increased colon cancer risk.
There is no known cure for Crohn's disease. Patients can manage symptoms with immunosuppressive medication or get temporary relief with surgery. If caught and treated early, and appropriately, Crohn's patients can better manage their symptoms and return to a relatively normal quality of life. What if doctors knew in advance which treatment would work best? That is, whether a patient should get medication or surgery, so that they could bring relief to Crohn's patients sooner?
University Hospitals Digestive Health Institute and Case Western Reserve University's Center for Computational Imaging and Personalized Diagnostics (CCIPD) are developing a radiographic enterographic treatment score that can help clinicians distinguish between mild and severe Crohn's.
“Predicting which Crohn's patient will or will not respond to a specific therapy can tell us who might need more aggressive treatment and who might need less aggressive treatment,” said Maneesh Dave, MD, MPH, Attending Gastroenterologist, UH Cleveland Medical Center and Assistant Professor of Medicine, Case Western Reserve University School of Medicine.
If clinicians can determine whether medications are unlikely to work for a particular patient with Crohn’s disease, they can recommend going directly to surgery instead and avoiding the major side effects associated with immunosuppressive medications.
“Patients with Crohn's undergo magnetic resonance enterography (MRE) routinely as part of their clinical care to evaluate disease status,” says Satish Viswanath, PhD, an assistant professor in the department of Biomedical Engineering at Case Western Reserve University. “We take that standard-of-care MRI, remove any patient identifying information, and utilize a process termed radiomics to extract relevant image features. We then apply machine learning to these features to predict whether the patient will respond to treatment or not.”
WHAT IS RADIOMICS?
Radiomics is an extension of computer-aided detection (CAD), although the two processes are quite different. CAD approaches are intended to provide a single answer, such as indicating the presence or absence of cancer. The radiomics process works by computing a large number of subtle image measurements from routine MRI, CT and PET images, capturing information that may not always be visible to the human eye. A researcher or data scientist then mines radiomic features to confirm or deny a hypothesis or to predict a particular outcome (e.g. response, survival).
Due in part to support from the National Cancer Institute, researchers have used radiomics most often for cancer detection, diagnosis, and prediction of response to treatment. Because radiomics uses standard-of-care images, researchers have access to mountains of data without any extra burden on the patient.
THE ROLE OF ARTIFICIAL INTELLIGENCE (AI)
CCIPD uses machine learning, deep learning and other approaches to analyze data to advance oncology and other disease treatment.
“Just like Netflix uses machine learning to suggest what movies to watch next, we are applying machine learning approaches to predict long-term outcomes for patients,” Dr. Dave says.
In addition to supporting research around Crohn's disease, CCIPD is using machine learning to better understand a number of different diseases including prostate, breast, colorectal, lung, and brain cancer, as well as cardiovascular and eye diseases. Several high-impact studies have been conducted to predict cancer aggressiveness, reduce overdiagnosis of cancer, and predict response to different therapies.
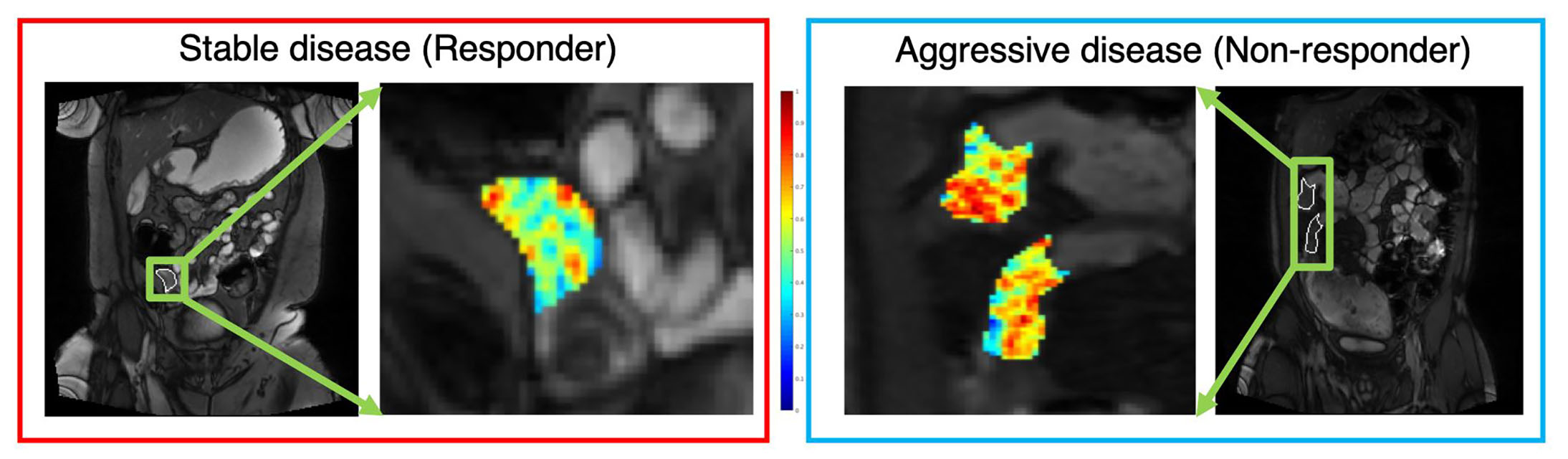 Image caption: Radiomic features extracted from MRE of a patient with mild disease and aggressive/severe disease
Image caption: Radiomic features extracted from MRE of a patient with mild disease and aggressive/severe disease
WHAT'S NEXT?
Crohn's is a frustrating disease for doctors and patients alike. Patients present with a variety of symptoms and complications. No one knows the exact cause, although several theories exist, and no single treatment works for everyone.
Medications currently used to treat Crohn's symptoms include aminosalicylates, corticosteroids, immunomodulators and biologic therapies. Doctors recommend surgery for complications such as fistulas, serious bleeding, intestinal obstructions and serious medication side effects. They may also consider surgery when symptoms don't improve with medication.
Surgical options for Crohn’s patients include bowel or intestinal resection or ostomy surgery, also known as bowel diversion. Upto 60 percent of Crohn’s disease patients require surgery within 20 years of having Crohn’s disease.1
Using advanced technology such as AI, machine learning and data science to advance treatment for various cancers, as well as to better understand chronic conditions such as Crohn's Disease, will be critical steps in establishing UH as a clinical leader in precision medicine. Identifying for an individual patient a marker of disease or predicting their response to a specific treatment could have a huge impact on patient care.
A long-range goal of the UH Digestive Health Institute is to work with CCIPD on a multicenter study, Dr. Dave adds. “We hope to conduct a much larger study to evaluate our radiomic score for Crohn's disease,” he says.
To refer a patient to a UH digestive health specialist, call 1 (800) 552-8338 or (216) 844-7553.
References:
- Peyrin-Biroulet L, Harmsen WS, Tremaine WJ, Zinsmeister AR, Sandborn WJ, Loftus EV Jr. Surgery in a population-based cohort of Crohn's disease from Olmsted County, Minnesota (1970-2004). Am J Gastroenterol. 2012 Nov;107(11):1693-701.
- Gillies RJ, Kinahan PE, Hricak H. Radiomics: Images Are More than Pictures, They Are Data. Radiology. 2016 Feb;278(2):563-77.


