UH, OSU Partner on Smart Diagnostic Tool for Pediatric Ear Pathology
October 15, 2018
UH Innovations in Otolaryngology - Head & Neck Surgery - Fall 2018
 Jay Shah, MD
Jay Shah, MDEach day in countless primary care offices and urgent care centers, first-line clinicians peek into the ears of fussy, wriggling patients to determine if they have acute otitis media (AOM). In fact, middle ear infection is the most commonly treated disease in children, resulting in a national annual healthcare cost estimated at $5 billion.
However, diagnosis of AOM via handheld otoscopy is clinically subjective and an abundance of caution has led to over-treatment and over-prescription of antibiotics. What if there was an objective tool to diagnosis not only AOM but other common pediatric ear conditions?
Jay Shah, MD, Pediatric Otolaryngology, UH Rainbow Babies & Children's Hospital, and Assistant Professor, Otolaryngology and Pediatrics, Case Western Reserve University School of Medicine is collaborating with researchers at The Ohio State University to pilot Autoscope smart digital technology to improve accuracy in the diagnosis of ear disease. The Autoscope otoscopy image analysis software is capable of detecting more than 14 eardrum abnormalities.
“Imaging technologies like ultrasound or CAT scan have become integral diagnostic tools for clinicians, but we haven’t had anything equivalent for the ear,” Dr. Shah says. “Developing a real-time solution for diagnosing ear pathology will have a national impact on enhancing patient care. We are fortunate that University Hospitals is a pilot site for the Autoscope project.”
Provisionally patented, Autoscope has two main objectives:
- to create enhanced composite images of the eardrum using novel computer vision and image stitching of otoscopic video clips gathered during patient examination, and
- to employ machine learning approaches to provide clinicians with automated identification of eardrum abnormalities.
Computer-assisted image analysis (CAIA) of composite images of the eardrum will generate a likely diagnosis and level of confidence for each patient, such as an 80 percent likely diagnosis of AOM. Previous studies have utilized CAIA but have been limited in focus to determining or ruling out AOM. In contrast, the Autoscope developers’ goal is to assist in point-of-care diagnosis of a number of ear pathologies, including AOM, middle ear effusion (non-infected fluid), cholesteatoma (skin cyst in the ear), eardrum perforation and eardrum retraction. Clinicians also will be able to search other cases from the well-annotated database and retrieve relevant eardrum images for comparison and diagnostic support.
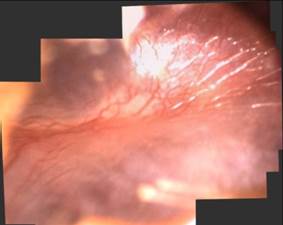 Digital image of normal appearing tympanic membrane.
Digital image of normal appearing tympanic membrane."My role is to spearhead video image collection at UH Rainbow Babies and Children’s Hospital to expand the database,” Dr. Shah says. “Ultimately, my hope is to not only help develop Autoscope, but also test and refine its accuracy.”
Dr. Shah will utilize a hand-held video otoscope system to record clips of patient eardrums and will also input annotations that document his evaluation of each case.
The existing Autoscope dataset of 600 patients will be augmented with video clips of left and right eardrums gathered from an additional 300 pediatric and 300 adult patients. Because it is essential for the CAIA approach, videos captured in the early phases of the project need to be well-focused and properly illuminated.

The optimal time for recording these high-quality images is when children are anesthetized for ear tube placement. “We can capture the images just prior to surgery when the patient is still and then further assess the ear in the operating room to determine a definitive diagnosis,” Dr. Shah says.
Additional images will be collected in ENT specialty outpatient clinics and primary care settings to represent “best possible” and “typical” clinical views of eardrums. As the registry of patients grows, researchers will continue to validate and refine the prototype algorithm, comparing diagnostic decisions of otolaryngologists with primary care clinicians and testing composite images against traditional handheld otoscopy.
To contact Dr. Shah regarding this initiative, Jay.Shah@UHhospitals.org.


