Blending Education with Technology
May 16, 2018
3D-printed models help UH residents learn critical surgical skills
UH Otolaryngology - Head & Neck Surgery - Summer 2018
 Sarah Mowry, MD
Sarah Mowry, MDPost-doctoral students and residents at the Case Western Reserve University School of Medicine Department of Otolaryngology – Head & Neck Surgery, are learning microdissection in a new and exciting way that will give them a distinct advantage in the operating room.
The learning method uses 3D-printed models of the temporal bone, and was introduced to the ENT Department by Sarah Mowry, MD, Associate Program Director, Department of Otolaryngology and ENT Institute, University Hospitals Cleveland Medical Center and Case Western Reserve University School of Medicine . Previously, Dr. Mowry demonstrated the educational effectiveness of images sourced from CT scans printed in acrylonitrile butadiene styrene (ABS) plastic filament on a MakerBot 2X 3D printer.
Far less expensive than cadaveric dissection (the 3D models cost just $1.92 each), this training tool provides valuable skill-building for learners and accurate assessment for instructors. Ultimately, patients benefit from surgical talent that has gained experience, as well as an understanding of, normal and pathological anatomy. The polymer models can be color-coded so that students learn how to navigate around surrounding tissue, blood vessels and nerves.
ESTABLISHING AN IMAGE LIBRARY FOR 3D MODELS
Through a $10,000 grant sponsored by the Graduate Medical Education (GME) Office at UH Cleveland Medical Center, and in conjunction with the UH Radiology Department, Dr. Mowry has begun building a resource library of CT-scanned images of various temporal bone pathologies. It is from these scans that models can be printed.
“For inexperienced surgical residents, congenital cases where the anatomy is distorted or displaced are particularly challenging,” Dr. Mowry notes. “Suppose a patient has cholesteatoma or contracted bone. The abnormal pattern of bone growth is very tricky for residents to drill. But once they have consistently demonstrated the skill, we are much more likely to allow them to perform a surgical procedure in the operating room.”
EVALUATING 3D MODELING TECHNOLOGY
In addition, the think[box] Student Project Fund has provided $2,500 grants for two UH studies related to the use of 3D-printed models.
Selecting the right 3D printer
The goal of the first study is to evaluate the quality of four different 3D printers to be used in the lab at UH. A panel of expert surgeons will rate the machines based on the compositional quality and detail of printed models, as well as purchasing and operational costs.
High-fidelity printers with many features and more flexibility can cost around $1 million, Dr. Mowry says, adding that her consumer-level, $350 desktop 3D printer has worked fine. Nonetheless, she would like to see a happy medium between fidelity and cost.
UH surgeons will compare two high-end printers from the Larry Sears and Sally Zlotnick Sears think[box], Case Western Reserve University's Center for innovation and entrepreneurship along with two lower-cost models.
 3D-printed models of a cadaveric temporal bone created on the various printers including (from left to right) Makerbot, Formlabs (2 different models), Fortus 400 and Objet.
3D-printed models of a cadaveric temporal bone created on the various printers including (from left to right) Makerbot, Formlabs (2 different models), Fortus 400 and Objet.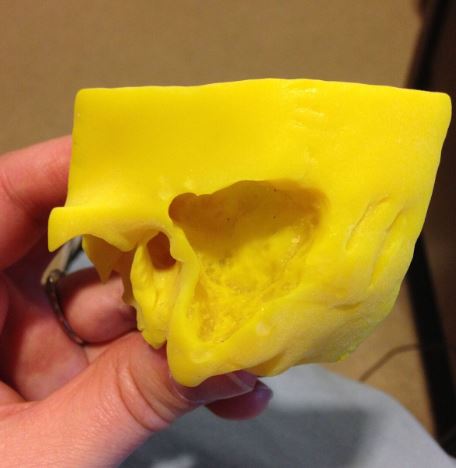
The resident comparison study
So, what constitutes skill mastery when it comes to drilling the human skull? That is what Dr. Mowry and her team hope to find out by studying 3D-printed “bones” used as a teaching tool for residents.
“Past studies have shown that residents need to drill 15-18 cadaver temporal bones to understand and get comfortable with demonstrating their ability to dissect safely and appropriately,” Dr. Mowry explains. “So, I wanted to see if the residents drill the same bone twice, can they improve on their performance the second time around? Or is it the learning curve?”
Likewise, if residents drill two different bones, will they make the same mistakes in each bone because the anatomy is different? “Is it the act of drilling that makes you better or is it beneficial to drill the same anatomy twice?” she says.
PREPARING THE SURGEONS OF TOMORROW
The trend toward using printed anatomical models has been picking up as cadavers from Willed Body Programs are becoming harder to get and more expensive, Dr. Mowry says. Another drawback is the limitations of cadavers when it comes to learning and applying specific techniques in cases of pathology because most cadavers have normal anatomy.
“It is a struggle when you take a resident who hasn’t had experience transferring their experience of normal anatomy to cases where pathology is present,” Dr. Mowry says.
The buzz around 3D models is attracting inquisitive minds to Dr. Mowry’s office door. From ideas about what pathologies to include in the image library to technological questions, enthusiasm is radiating.
“The residents love this blend of education and technology, which is a hot topic right now,” Dr. Mowry explains. “They are always fun to work with because they ask, ‘Should we try this?’ and I reply, ‘Why not?’”
The use of 3D modeling makes learning surgical techniques fun, and it helps ensure that tomorrow’s surgeons will be confident and highly skilled. By embracing the technology, the Department of Otolaryngology – Head & Neck Surgery is well-positioned to offer residents an engaging and useful learning experience.


