Controversies In Cardiology
January 30, 2017
Harrington Heart & Vascular Institute Innovactions – Winter 2017 – View Full PDF
Daniel Simon, MD: It is my privilege to welcome Dr. Joseph Sabik to our Controversies in Cardiology series. Joe is one of the nation’s leading heart surgeons and has joined University Hospitals as the Chairman of the Department of Surgery. He was most recently Chairman of Thoracic and Cardiovascular Surgery at the Cleveland Clinic and has performed more than 8,000 heart operations. His areas of clinical expertise include multi-arterial coronary artery bypass grafting, minimally invasive heart surgery, and heart valve repair and replacement surgery. Joe is clearly an expert for our topic today: PCI or bypass surgery for left main coronary artery disease.
Joseph Sabik, MD: Thank you, Dan. I am really excited to be joining UH and the Harrington Heart & Vascular Institute. I also enjoy squaring off with an interventional cardiologist on the topic of optimal revascularization strategies for coronary artery disease.
Dr. Simon: So let’s set the stage for our readers and listeners. Patients with obstructive left main coronary artery disease are usually treated with CABG. Randomized trials such as SYNTAX have suggested that drug-eluting stents may be an acceptable alternative to CABG in selected patients with left main coronary artery disease. We just returned from the TCT in Washington, DC, and heard the results of the landmark EXCEL trial that was also published in the New England Journal of Medicine. You are one of the Co-PIs of this trial. Congratulations. Tell me about the design of the trial.
Dr. Sabik: EXCEL is a large, multinational, multicenter trial that randomized 1,905 patients with left main coronary artery disease of low or intermediate anatomic complexity to undergo either PCI with a Xience everolimus-eluting stent or CABG. Anatomic complexity was assessed at the site and included patients with a SYNTAX score of 32 or lower. The primary endpoint was the rate of the composite endpoint of all cause death, stroke or MI at three years, and the trial was powered for noninferiority testing of the primary endpoint. Secondary endpoints included the same composite at 30 days as well as the addition of ischemia-driven revascularization at three years. Importantly, patients had to be suitable for revascularization by either strategy of revascularization by a heart team that included both a heart surgeon and interventional cardiologist. The goal of PCI or CABG was to achieve complete anatomic revascularization.
Dr. Simon: It is important to add that the trial tested contemporary PCI and surgical techniques. The Xience stent has a very low rate of stent thrombosis and restenosis. Tell me about surgical recommendations.
Dr. Sabik: We encouraged the use of arterial bypass grafts, intra-operative epi-aortic as well as trans-esophageal echocardiography. On- or off-pump CABG was performed at surgeon’s discretion. On average, 2.6 grafts per patient were placed and an internal thoracic artery graft was used in nearly 99 percent of the patients. Bilateral ITA grafts were used in nearly 29 percent of patients and radial artery grafts in 6 percent. All arterial grating was performed in 25 percent. In the PCI arm, 2.4 stents with an average total stent length of 49 mm were implanted per patient.
Dr. Simon: As an interventional cardiologist who performs unprotected left main procedures, it is also worth mentioning that distal left main bifurcation or trifurcation disease was present in 80 percent of the patients, and two-vessel or three-vessel disease was present in 51 percent of the patients. So, what are the top-line results?
Dr. Sabik: The incidence of the primary endpoint of death, stroke or MI at three years occurred in 15.4 percent of patients in the PCI group and in 14.7 percent of patients in the CABG group with a hazard ratio of 1.0. This enables us to conclude that PCI was noninferior to CABG with respect to the primary endpoint. The secondary endpoint of death, stroke, MI and ischemia-driven revascularization occurred in 23.1 percent of patients in the PCI group and in 19.1 percent of patients in the CABG group, achieving noninferiority but not reaching statistical significance for superiority.
Dr. Simon: In general, the purpose of a noninferiority trial design is to determine whether a new device, drug or treatment strategy that might offer safety or quality of life advantages is still efficacious. In other words, is there a trade-off that one is willing to accept? In EXCEL, this tradeoff was set as a noninferiority margin of 4.2 percent. Therefore, it is worth looking at the early 30-day time point and landmark analysis to gain insight into the possible advantages of one strategy versus another.
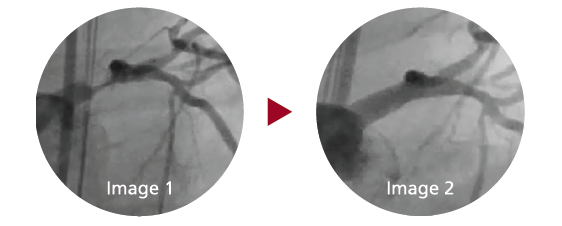
Image 1: 72 M hx of TIA presenting for concern of three hours of chest pain at rest, 7/10. Coronary angiogram reveals 90 percent left main stenosis and chronic total occlusion of the RCA.Patient was considered a high-risk candidate for CABG and decision for PCI with circulatory support, Impella 2.5 L made. Image 2: Result after a single drug-eluting stent in the left main 3.5 x 15 mm, post-dilated with a 4.5 mm balloon. The Impella was removed at the end of the procedure and the patient was discharged the next day in excellent condition.
Dr. Sabik: That is a great point. Indeed, in EXCEL we see that the secondary endpoint of death, stroke, or MI at 30 days occurred in 4.9 percent of PCI patients and in 7.9 percent of CABG patients, and this difference was highly statistically significant for superiority of PCI. In fact, other peri-procedural adverse events occurred less frequently in PCI compared to CABG patients: 8.1 percent versus 23 percent. PCI
patients experienced fewer major arrhythmias, fewer infections and fewer blood transfusions. However, the tide reversed in the landmark analysis after 30 days. Between30 days and three years, more primary endpoint events, particularly death and MI, occurred in PCI patients than CABG patients. Ischemia-driven revascularization was also higher in the PCI group than in the CABG group (12.6 percent versus 7.5 percent of the patients).
Dr. Simon: So the take home message from EXCEL is that the majority of patients with unprotected left main coronary artery disease, who are candidates for either procedure, can now be managed equally well by PCI or CABG with experienced interventional cardiologists and heart surgeons working in a collaborative heart team approach. Left main coronary artery disease may turn out to be a great example of personalized medicine. From the registry portion of the EXCEL trial, we learned that approximately 62 percent of patients with left main coronary artery disease are candidates for PCI, and approximately 80 percent are eligible for CABG. Therefore, decisions to proceed with PCI or CABG should be made by the heart team and patient taking into account the patient’s anatomy, comorbidities and preferences.
Dr. Sabik: I think it is really critical for us to emphasize the importance of further follow-up of the patients at five years given the landmark analysis indicating increased events in the PCI cohort after 30 days. The presentation of the NOBLE trial at the same late-breaking clinical trials session at the TCT indicates that long-term follow-up is essential. Indeed, NOBLE concluded that PCI was inferior to CABG at five years. Although there are many trial design and device differences between EXCEL and NOBLE that may be responsible for the divergent outcomes of the two trials, we should encourage our readers and listeners to keep an eye out for the five-year EXCEL results.
Dr. Simon: Joe, thank you for your leadership in the EXCEL trial and your insights into the trial results. As classmates at Harvard Medical School, I can’t tell you how thrilled I am to be working with you again after all these years. I know that you will play a leading role in driving our mission – To Heal. To Teach. To Discover. – as our Chair of Surgery at University Hospitals.

DANIEL I. SIMON, MD
President, University Hospitals
Professor of Medicine
Case Western Reserve University School of Medicine
JOSEPH F. SABIK, III, MD Chair
Department of Surgery, University Hospitals
Cleveland Medical Center
Surgeon-in-Chief and Vice President of Surgical
Operations, University Hospitals
Professor of Surgery, Case Western Reserve University
School of Medicine
Tags:


