Endonasal Excellence
January 01, 2016
Rare surgery results in great outcome for young NF-2 patient
Innovations in Otolaryngology - Head and Neck Surgery Winter 2016 Download PDF
 Kenneth Rodriguez, MD
Kenneth Rodriguez, MD
Neurofibromatosis type 2 (NF-2) is an autosomal dominant syndrome with multiple manifestations, most notably neurologic lesions. “It’s rare for masses to develop in the pterygopalatine fossa or infratemporal fossa, but given the neural structures in those regions, it certainly can occur,” says Kenneth Rodriguez, MD, Chief of Allergy, Rhinology/Anterior Skull Base Surgery; University Hospitals Cleveland Medical Center and UH Ear, Nose & Throat Institute; Assistant Professor of Otolaryngology, Case Western Reserve University School of Medicine.
Dr. Rodriguez was presented with such a case in April 2015 – a young man with NF-2 who’d previously had surgery at another hospital to remove one of his bilateral acoustic neuromas. The patient complained of left facial pain and pressure, nasal airway obstruction, decreased sense of smell and epistaxis. Imaging demonstrated a left infratemporal fossa/pterygopalatine fossa mass, consistent with a schwannoma.
“It had remodeled the medial wall of the pterygopalatine fossa and floor of the orbit,” Dr. Rodriguez says. “It had expanded posteriorly to be lateral to the left sphenoid sinus at the base of the temporal lobe.”
Based on these findings and the patient’s symptoms, Dr. Rodriguez recommended surgery as the best option.
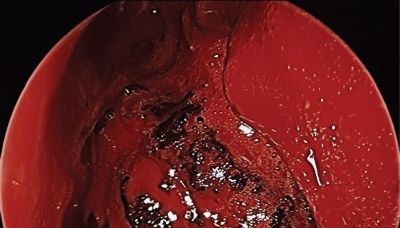 Endoscopic view of the left nasal cavity. The inferior turbinate has been resected, the maxillary sinus has been opened widely, and the ethmoid cavity has been dissected. The mass is centered within the pterygopalatine fossa with expansion in all orientations.
Endoscopic view of the left nasal cavity. The inferior turbinate has been resected, the maxillary sinus has been opened widely, and the ethmoid cavity has been dissected. The mass is centered within the pterygopalatine fossa with expansion in all orientations.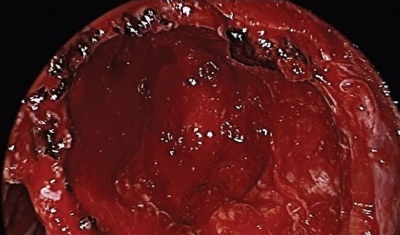 Post resection view. The posterior wall of the maxillary sinus has been widely opened. Posterioinferiorly are the pterygoid plates and superiorly the lesion was in close approximation to the temporal lobe. Within the anterior superior region of the resection cavity the orbit is dehiscent. The internal maxillary artery was identified and preserved inferiorly.
Post resection view. The posterior wall of the maxillary sinus has been widely opened. Posterioinferiorly are the pterygoid plates and superiorly the lesion was in close approximation to the temporal lobe. Within the anterior superior region of the resection cavity the orbit is dehiscent. The internal maxillary artery was identified and preserved inferiorly.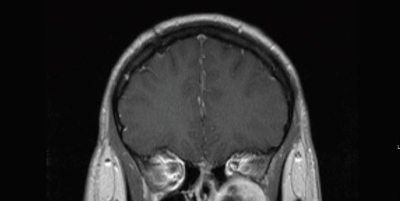 Coronal T1 post contrast MRI demonstrating the left sided schwannoma centered within the pterygopalatine fossa. Inferior orbital compression is demonstrated.
Coronal T1 post contrast MRI demonstrating the left sided schwannoma centered within the pterygopalatine fossa. Inferior orbital compression is demonstrated.“Although the lesion appeared radiographically benign, it was likely going to continue to slowly grow over time and cause progression of symptoms,” Dr. Rodriguez says. “What makes these tumors very interesting is that they slowly expand and can displace normal structures. Given the proximity to his orbit, he could begin to experience double vision as his eye was slowly displaced superiorly. There was also a small chance of the lesion degrading into malignancy.”
To resect the tumor, Dr. Rodriguez and his team opted for an endonasal approach. “Normal endoscopic sinus surgery is all about preserving normal structures,” Dr. Rodriguez says. “The problem is when you’re doing tumor surgery, you need wide access. If you get into bleeding, you can’t be in a limited space especially with vessels like the internal maxillary artery. To gain wide exposure, we did an endoscopic medial maxillectomy approach involving resection of the inferior turbinate, lacrimal bone and medial maxilla to be able to take a 0 degree scope, put it in the nostril, turn it to the side and see the entire back wall of the maxillary sinus straight on.
“When the tumor was grossly resected, the patient’s orbital floor was basically free-floating because of bone loss from compression by the tumor,” Dr. Rodriguez adds. “However, with the periorbita intact, his eye maintained normal position following resection.”
There was no leak of cerebrospinal fluid following surgery, and the internal maxillary artery was identified and was left intact. His pathology was schwannoma, and following recovery, the patient’s symptoms resolved. He did not develop “empty nose syndrome,” which can occur after aggressive endonasal surgery, and he did not develop numbness of V2. However, the patient does have some numbness on the left side of his hard palate.
“This makes us suspect the tumor may have originated from one of the sensory nerves going to the hard palate,” Dr. Rodriguez says. “It is very gratifying to be able to remove such a large mass via endonasal techniques with minimal morbidity.”
For more information on this case, email Kenneth.Rodriguez@UHhospitals.org.
Tags:


