Our History
History and Development of the Department of Ophthalmology & Visual Sciences and Visual Sciences Research Center (VRSC)
The Department of Ophthalmology at University Hospitals Cleveland Medical Center and Case Western Reserve University (CWRU) was formally established as an independent department in 1991. Previously, the eye care needs of University Hospitals for its 150 year history, were served by the ophthalmology faculty who were a Division of the Department of Surgery. In 1995, the Department received Research to Prevent Blindness Foundation (RPB) funding which served as a major catalyst for the growth and development of the research mission. In 2004, the name of the Department was changed by the University to the Department of Ophthalmology & Visual Sciences in recognition of its broader mission of basic and translational research in the visual sciences. Dr. Jonathan Lass, the first chair of the Department, stepped down as Chair in 2013 after 20 years, and Dr. Douglas Rhee was appointed Department Chair in September 2013, bringing clinical and research expertise in glaucoma.
With support from UH Cleveland Medical Center and CWRU School of Medicine, Dr. Lass expanded the basic research in the Department and founded the Visual Sciences Research Center (VSRC) with seven other basic science and clinical departments in the School of Medicine in 1996. The next year, the VSRC obtained its first National Eye Institute (NEI) Core Grant (P30 EY11373) with Dr. Lass as Principal Investigator for the first 10 years of funding. An NEI Institutional Training Grant (T32 EY07157) subsequently was obtained in 2000 based on the strength of its senior scientists and their training record leading to the establishment of the CWRU Visual Sciences Training Program (VSTP). These two grants along with the RPB unrestricted funding and individual awards have been the foundation for the research programs within the Department and larger VSRC. In essence, the Department once receiving unrestricted RPB funding drove the growth of the visual sciences throughout the School of Medicine and beyond to Biomedical Engineering and even Chemistry, an undergraduate department.
Our investigators, laboratory and clinical, have made significant and important contributions to the fundamental understanding of vision, ophthalmic disease, and the care of ophthalmic patients.
Major Research Achievements in Our History
1945 – Charles I Thomas, MD, performed the first corneal transplant in Northeast Ohio, paving the way to restored vision for millions of people. In 1958, he established the Cleveland Eye Bank (now Eversight Ohio).
1961 – Albert Potts, MD, PhD, received the Association of Research in Vision and Ophthalmology’s highest award, the Friedenwald Award, for his studies of alcohol toxicity on the optic nerve, which helped advance the understanding of how the optic nerve works.
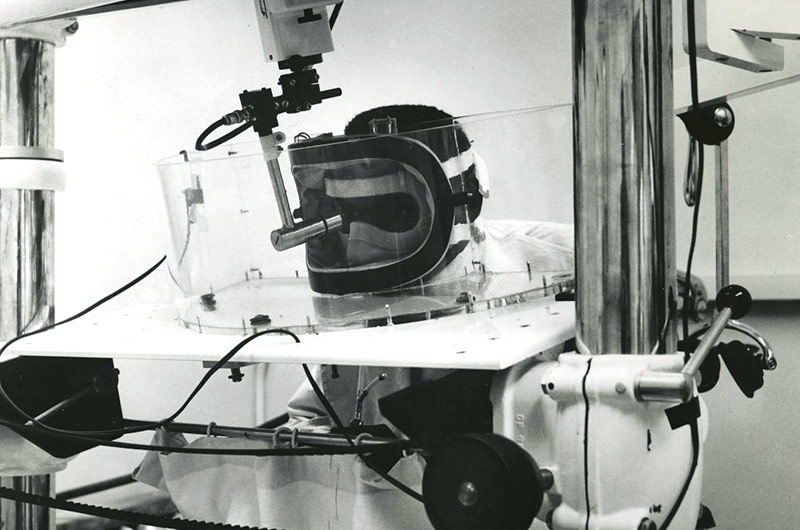
1966 – Edward Purnell, MD, led a team of researchers that pioneered the use of ultrasound to study the eye and diagnose eye diseases and developed ultrasound techniques for eye surgery that revolutionize common procedures such as cataract removal. In 1972 he developed the first hand-held ultrasound device for the eye.

1999 – Edward Kean, PhD summarized his seminal work on the dolichol pathway in the retina and its involvement in the glycosylation of rhodopsin furthering our understanding of the biochemistry of vision.
2002 – John Porter, PhD published a review of his work on extraocular muscle cellular adaptations for a diverse functional repertoire furthering our understanding of the complex actions of the extraocular muscle normally and in disease.
2002 – Eric Pearlman, PhD, Jonathan Lass, MD, and their team discovered the bacteria, Wolbachia, facilitates the inflammatory response associated with the disease of sub-Saharan Africa known as river blindness or onchocerciasis caused on Onchocerca volvulus. Their work led to the use of antibiotics to treat this disease, a totally new approach.
2001, 2006 – Douglas Rhee, MD, is one of the first to describe a bilateral acute angle closure caused by a commonly used medication, topiramate. Later, he discovered the accepted treatment for the intractable form of this disease.
2005 – Douglas Rhee, MD, becomes the fifth surgeon in the world and only surgeon outside of California to perform the trabectome procedure which would later become known as the first minimally invasive surgery for glaucoma helping to usher in a new era of minimally invasive glaucoma surgery.
2006 – Douglas Rhee, MD, discovers that the uncommon cause of narrow angle glaucoma, plateau iris syndrome, has an autosomal dominant inheritance pattern in approximately half of patients affected.
2007 – Loretta Szczotka-Flynn, OD, PhD was the first to publish epidemiologic findings on risk of corneal inflammation with certain contact lens materials. Since then, her findings have been corroborated around the world and her subsequent studies led to finding specific risk factors leading to corneal inflammation with contact lens wear including bacterial bioburden present on worn contact lenses or patient lid margins.
2008 – Faruk H. Örge, MD, was the second in the nation and first in Ohio to use endoscopic and microsurgical techniques to drain excess fluid from the eye in infants and young children born with glaucoma. He also was the first in Northeast Ohio to use a new class of drugs (anti-VEGF) to treat retinal disease in premature infants.
2012 - 2019 – Irina Pikuleva, PhD, along with her colleagues in the laboratory showed that cholesterol metabolism in the retina is important for normal retinal structure and function and that retinal cholesterol dyshomeostasis leads to pathologic changes in retinal and choroidal blood vessels.
2013 – Douglas Rhee, MD, advanced new surgical techniques for management of severe glaucoma, including introducing Trabecutome surgery to Northeast Ohio, a less-invasive approach to filtration surgery.
2013 – Jonathan Lass, MD along with his colleagues, William Reinhart, MD; and Beth Ann Benetz, MA, CRA, FOPS, was one of the leaders in a National Eye Institute funded study, the Cornea Donor Study, demonstrating that donor age is not a significant factor in the success of corneal transplantation, which expands the pool of available tissue by including older donors.
2014 – Faruk H. Örge, MD obtained the patent for a novel minimally invasive glaucoma device to by-pass trabecular meshwork and re-facilitate the aqueous humor flow from the anterior chamber to the Schlemm’s canal.
2017-19 – Jonathan Lass, MD along with his colleagues Ms. Benetz and Loretta Szczotka-Flynn OD, PhD led the National Eye Institute funded study, The Cornea Preservation Time Study, that found that donor corneas can be stored 3-4 days longer prior to transplantation than current practice improving the distribution of donor tissue worldwide and assuring quality.
2018 – Faruk H. Örge, MD filed patent on 3 dimensional ocular ultrasonography and on its various applications with a diverse team of CWRU engineers.


