Compassionate, Comprehensive Care for Patients with COVID Long-Haul Syndrome
Recent studies have shown that 20 – 30 percent or more of individuals infected with COVID-19 will continue to have health problems for weeks, even months, after their body has cleared the virus. The University Hospitals COVID Recovery Clinic is dedicated to the comprehensive evaluation, diagnosis and multidisciplinary treatment of patients with Post-Acute Sequelae of SARS-CoV-2 infection (PACS), more commonly referred to as COVID Long-Haul Syndrome.
Schedule an Appointment
If, after your acute course of COVID-19, you are still experiencing symptoms, call us today at 216-966-9000 to schedule an evaluation.Advanced Multidisciplinary Expertise for Optimal Outcomes
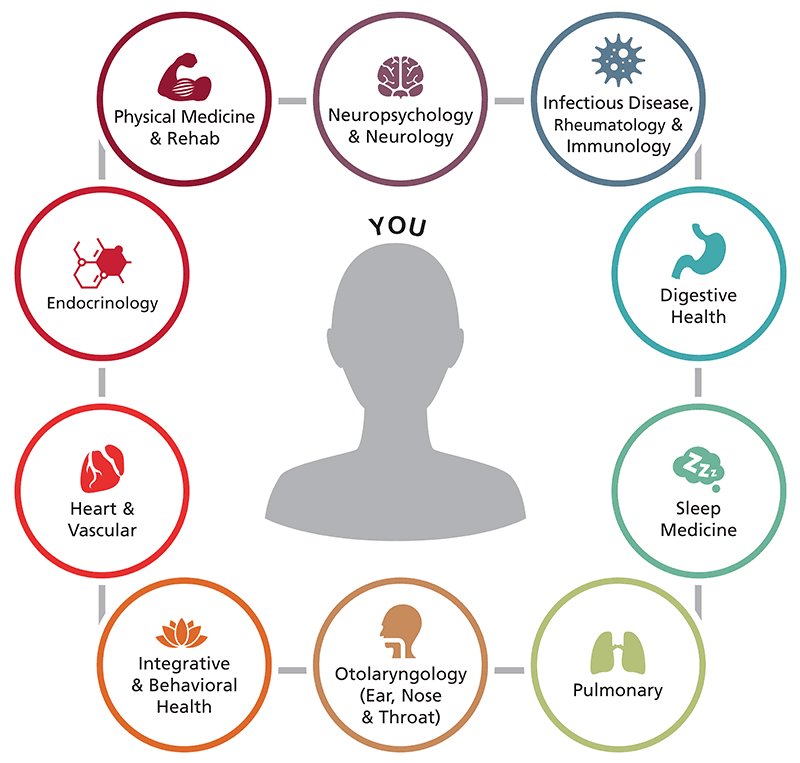
Patients with COVID Long-Haul Syndrome often seek medical help but their symptoms are not recognized as being COVID-related, so they don’t receive the coordinated, multidisciplinary care they need. At the UH COVID Recovery Clinic, patients have access to a vast network of medical specialists with the training and experience to recognize the syndrome, perform the appropriate diagnostic tests, and develop a personalized treatment plan to address every physical and behavioral aspect of the patient’s illness, which may include the following symptoms:
- Shortness of breath, coughing and fever
- Fatigue and exhaustion
- Brain fog
- Atypical chest pain and palpitations
- Behavioral health issues like depression and anxiety
- Difficulties with cognition and memory
- Insomnia and other sleep problems
- Generalized pain and muscle aches
- Joint pain and impaired mobility
- Persistent loss of smell and taste
- Headache
- Diarrhea
- Skin rashes
The multitude of complaints listed above reflect how COVID Long-Haul Syndrome can affect multiple organ systems in the body, including the pulmonary, hematologic, cardiovascular, neuropsychiatric, renal, endocrine, gastrointestinal/hepatobiliary and dermatologic systems. The impact on patients’ health can range from mild to severe with the latter being totally debilitating.
Creating Personalized Pathways to Healing
Located at UH Ahuja Medical Center, the UH COVID Recovery Clinic offers both in-person and virtual care based on the patient’s specific symptoms and needs. Our goal is to identify the best way(s) to manage your symptoms and coordinate the multidisciplinary care required to restore your health. Care will be individualized for you as a whole person - both mind and body - and designed to help you return to the activities you love. Patients can schedule an appointment directly with the UH COVID Recovery Clinic or may be referred for an evaluation by their primary care provider.
Scheduling Appointments and Medical Questionnaires
Once you have scheduled an appointment, you will be emailed or mailed a medical questionnaire to complete and send back. This questionnaire will ask you to provide details about your COVID history (dates, symptoms and treatments received) along with a description of your current symptoms and other health issues as compared to your functioning status prior to COVID.
Once we have your completed questionnaire, the patient journey will be as follows:
Initial Assessment
At the initial evaluation (in person or virtually) you will meet with our specially trained nurse practitioner who will review your questionnaire and ask additional questions designed to screen for depression, anxiety, sleep disturbances, fatigue, cognitive deficits and more. You will also be asked about your current symptoms, day-to-day activities, medical history and the medications you are taking. For those being seen in person, the nurse practitioner will perform a physical examination.
Based on the findings of the initial assessment, the nurse practitioner, in collaboration with the UH COVID Recovery Clinic’s medical director, David M. Rosenberg, MD, MPH, will develop a care path for each patient. This care path will often include input from individual members of our multispecialty panel. Your care will be approached as a team effort in order to guide your pathway to recovery.
Personalized Diagnostic Testing
An accurate diagnosis is essential for a successful treatment plan. Based on the information collected during the initial assessment, and on the recommendation of the specialists on the patient’s care team, a variety of diagnostic tests may be ordered. These may include but are not limited to:
- Pulmonary function testing
- Imaging tests that may include computed tomography (CT) scans and magnetic resonance imaging (MRI)
- Cardiovascular testing including electrocardiogram (EKG) and/or event monitoring, echocardiogram, stress testing
- Laboratory testing
- Sleep studies
- Neuropsychological testing
- Testing for autonomic dysfunction
Collaborative, Multidisciplinary Team Approach to Care
Based on the patient’s specific symptoms and the care plan developed by the nurse practitioner and medical director, referrals for specialty consultation may be deemed appropriate. These types of referrals will help customize the treatment team for a given patient. Potential specialty areas for referral include:
- Pulmonary
- Pulmonary
- Heart & Vascular
- Sleep Medicine
- Behavioral & Integrative Health
- Neurology & Neuropsychology
- Rheumatology, Infectious disease & Immunology
- Otolaryngology (ENT)
- Digestive health
- Endocrinology/Metabolic Health
Treatment Plan and Follow-Up Care
Your on-going care surrounding COVID will be managed by your team at the UH COVID Recovery Clinic and regular follow-ups with our nurse practitioner will be scheduled. The nurse practitioner will help coordinate recommendations received by your care team, namely that provided by given specialists or those providing specific treatment. All information pertaining to your care surrounding COVID will be forwarded directly to the UH COVID Recovery Clinic’s electronic data base, ensuring that our staff is always up-to-date on the care you have received.
To monitor and track your progress over time, we will occasionally ask you to update us with details about your treatment, symptoms and overall path to recovery. Your team at the UH COVID Recovery Clinic will use this data to help define the natural history of COVID Long-Haul Syndrome and advance much-needed research related to the diagnosis, symptoms and treatments for this syndrome.
COVID-19 Recovery & Longhauler Clinical Study
The University Hospitals Clinical Research Center is conducting an observational research study about COVID-19 (also known as SARS-CoV2) to learn more about long-term effects of COVID-19, and who is at greatest risk. To learn more, visit the COVID-19 Recovery & Longhauler Study.
Integrated, Whole-Person Care
The UH COVID Recovery Clinic stresses the importance of treating the whole person. Whole-person care places an emphasis on integrative heath (stress management, relaxation techniques, acupuncture); behavioral health intervention for depression and anxiety or other psychological issues; rehabilitation services (PT, OT, neuropsychological rehabilitation); general pain management; and pulmonary/cardiac rehabilitation. In addition, we know that patients recovering from COVID often have sleep disturbances, which can lead to general symptoms of fatigue, weakness and cognitive impairment. Therefore, patients at the clinic will also be evaluated for sleep-related health issues and prescribed the appropriate therapies to improve their sleep.
The multidisciplinary team of COVID care providers described below will meet regularly to discuss cases. These discussions will help to ensure that the diagnostic and therapeutic approach to caring for each patient is optimized.
COVID Long-Haul Syndrome in Pediatric Patients
Although initial research suggests that fewer children than adults develop COVID Long-Haul Syndrome, there have been reported cases of persistent, often debilitating post-infection symptoms in pediatric patients. These may include diarrhea, extreme fatigue, stomach pain, new onset headache or migraine, and chronic, recurring fever.
The pediatric specialists at UH Rainbow Babies & Children’s Hospital have an assessment and treatment model for children that is similar to the adult COVID-19 Recovery Clinic.
If your child had COVID-19 and is now experiencing symptoms of COVID Long-Haul Syndrome, call 216-966-8000 to speak to our nurse navigator. Pediatric patients with suspected post-infection syndrome will be referred to Amy Edwards, MD, pediatric infectious disease specialist at UH Rainbow Babies & Children’s Hospital.
Contribute to COVID-19 Research
When you report and seek treatment for your COVID Long-Haul symptoms, not only are you getting the help you need to feel better, you are helping the medical community learn more about the long-term side effects of COVID-19. Over time, this will help doctors find more effective ways to detect and treat both acute COVID-19 infections and COVID Long-Haul Syndrome.
Participation is voluntary and all patient information is kept strictly confidential.
Schedule an Appointment
If, after your acute course of COVID-19, you are still experiencing symptoms, call us today to schedule an evaluation at
216-966-9000