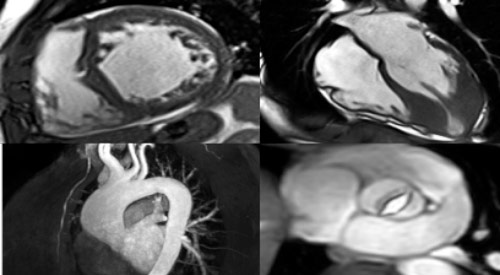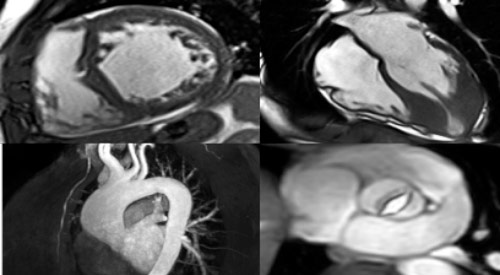
Cardiovascular MRI is a noninvasive test used to help diagnose or monitor heart and vascular disease. This scan uses powerful magnets to produce detailed pictures of the heart and surrounding blood vessels. MRI does not use ionizing radiation (x-rays). During the scan, you may receive contrast material to enhance the imaging, which helps to identify specific diseases.
You may have a cardiovascular MRI as an outpatient appointment or as part of your stay in the hospital. This test may be performed to:
- Evaluate the anatomy and function of the heart muscle, heart valves, major vessels and surrounding structures such as the pericardium (sac that surrounds the heart.)
- Identify diseases of the heart muscle including cardiac tumors, inflammatory and infiltrative conditions.
- Evaluate the effects of coronary artery disease such as reduced blood flow to heart muscle or scarring within the heart muscle after a heart attack.
- Plan patient treatment for a cardiovascular disorder.
- Monitor the progression of certain cardiac disorders over time.
- Evaluate the anatomy of the heart and blood vessels in children and adults with congenital heart disease.
Cardiovascular MRI poses almost no risk to the average patient when appropriate safety guidelines are followed. If contrast dye is used, there is a slight risk you may have an allergic reaction to the dye. Tell your doctor if you:
- Have ever had a reaction to contrast dye. Such reactions are usually mild and easily controlled by medication.
- Have severe kidney failure. Although Gadolinium contrast is extremely safe an extremely rare, complication may occur but only in patients with very poor kidney function.
- Are pregnant, think you may be pregnant or are breastfeeding.
You will complete an MRI Safety Checklist. Tell the technologist if you have ever had a reaction to contrast material. Report any medical or electronic devices in your body, metallic implants or metal under the skin. Many implants are compatible with MRI scans, but in some cases, it is not advised.
Inform your technologist of the following:
- Implanted pacemaker or defibrillator
- Cerebral aneurysm clip (from previous brain surgery)
- Metal in the eye
- Implanted nerve stimulator, insulin or narcotic pump
- Pregnancy (or you think you may be pregnant)
- Cochlear implant
- Vascular stents
You will remove your clothing, any metal objects (jewelry, bobby pins, eyeglasses, etc.), and be given a gown to wear. The technologist will scan you with a metal detector prior to entering the scanner.
The technologist or nurse will place an intravenous (IV) catheter in your hand or arm. If contrast material will be used, it will be injected through the IV during the scan.
Electrocardiogram leads will be placed on your chest to monitor the heart’s electrical activity during the scan.
During the MRI, you will be positioned on an examination table. A thin device containing the MRI sensor (coil) will be placed on your chest and held in position with loose fitting straps. The table is then moved into the MRI unit, an open-ended, wide-bore, fully lit and ventilated tube.
You will communicate with the technologist via an intercom (headphones with microphone) and be given a hand-held device to initiate communication with staff at any point during the scan. There is also a camera adjacent to the MRI allowing the technologist to see you during the scan.
The technologist will give you breathing instructions. You will hold your breath for short periods of time and be asked to remain still. The MRI may produce loud banging noises, which are shielded by earplugs and headphones.
A cardiovascular MRI can take 30 to 90 minutes, varying according to the type of scan ordered.
A cardiologist or radiologist will interpret your MRI scan and provide a report to your referring or primary doctor. A follow-up appointment with your doctor may be necessary to review the results of your scan.
If contrast material was used during your MRI scan, you may be watched for a period of time for any reactions. These include itching, swelling, rash or trouble breathing.
Contact your doctor if you notice any pain, redness or swelling at the IV site after returning home. These could be signs of an infection or other type of reaction.
You may resume your usual diet and activities unless your doctor tells you differently.