How Blood Cholesterol Levels Affect Your Health
Cholesterol is a naturally occurring fatty, waxy substance that is carried in the bloodstream to all the cells of the body. Manufactured in the liver, cholesterol is essential for many important bodily functions including the formation and maintenance of cell membranes. Too much cholesterol, however, can lead to health problems.
Make an Appointment
If you have a cholesterol-related health condition, the experts at UH Harrington Heart & Vascular Institute can help. Call 440-613-2388 to schedule an appointment today.
Find a CardiologistCholesterol-Related Conditions
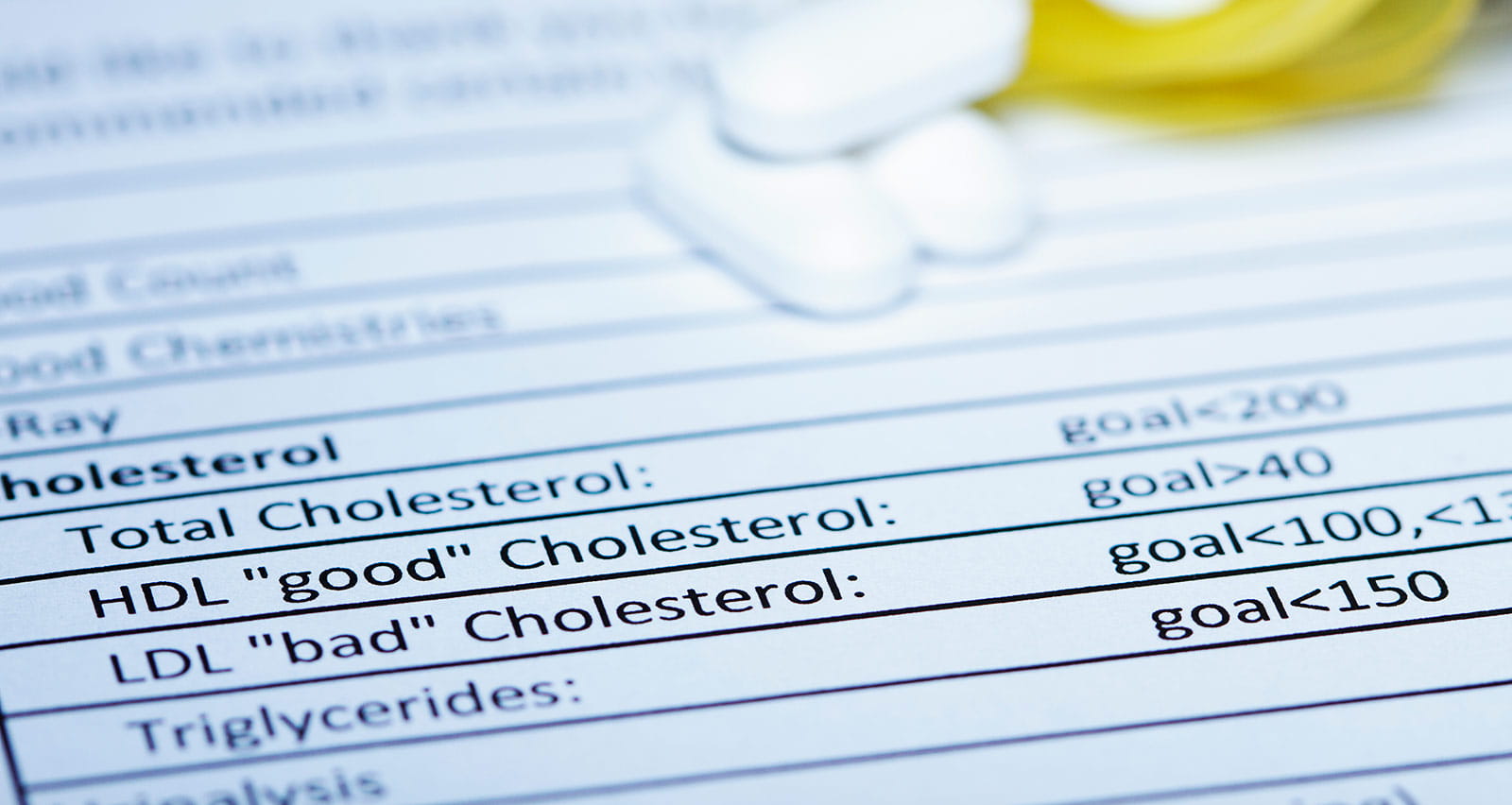
Total cholesterol (TC) is the total amount of cholesterol in the blood. It is made up of:
Low density lipoproteins (LDL). Often referred to as “bad” cholesterol, too much LDL cholesterol can cause a buildup of plaque in the arteries and lead to many serious health conditions.
High density lipoproteins (HDL). Often referred to as “good” cholesterol, high levels of HDL cholesterol are associated with a lower risk of heart disease, stroke and other cardiovascular conditions. Low levels of HDL may increase the risk for these conditions.
Triglycerides. The most common type of fat found in the bloodstream, triglycerides are a primary source of energy for the body. At high levels, it can contribute to plaque buildup in the arteries and increase the risk of heart disease and stroke.
Diagnosis of Cholesterol-Related Conditions
Although they can have serious health implications, abnormal blood levels of LDL, HDL and triglycerides rarely have symptoms. The only way to accurately diagnose cholesterol-related conditions is through a fasting blood test called a full lipid profile.
Lipid profile screenings typically begin in early adulthood and continues throughout life, often as part of an annual physical exam. The frequency of testing will vary depending on baseline findings and your risk factors for heart disease, including family history.
| TC | LDL | HDL | TG | |
|---|---|---|---|---|
 Dangerous: High/Very High |
≥240 mg/dL | ≥160 mg/dL
(high) ≥190 mg/dL (very high) |
<40 mg/dL
(male) <50 mg/dL (female) |
200-499 mg/dL
(high) ≥500 mg/dL |
 At Risk: Borderline High |
≥240 mg/dL | 100-159 mg/dL | 40-59 mg/dL
(male) 50-59 mg/dL (female) |
150-199 mg/dL |
 Heart-Healthy: Desirable |
≥200 mg/dL | <70 mg/dL Recommended for those with CAD or at very high risk: <55 mg/dL | ≥60 mg/dL | <150 mg/dL |
Make an Appointment
Helpful Resources for Patients
University Hospitals offers helpful insights and management strategies for patients with blood cholesterol conditions including high LDL, low HDL, high triglycerides and other associated health conditions.


