Wolff-Parkinson-White Syndrome
What is Wolff-Parkinson-White syndrome?
Wolff-Parkinson-White syndrome (WPW) is a type of heart condition you are born with (congenital). It causes a rapid heart rate. You may have episodes of palpitations or rapid heartbeats if you have WPW. WPW affects less than 1 in 100 people.
Normally, electrical signals travel through your heart in an organized way to control your heartbeat. This allows blood to pass from the upper chambers of your heart (the atria) to the lower chambers (the ventricles). It then travels out to your body. The upper and lower heart chambers are normally connected by a single main circuit in the center of the heart through which electricity flows. In WPW, there is an extra connection between the upper and lower chambers that can make you susceptible to arrhythmias that cause rapid heart rates (tachycardia).
What causes Wolff-Parkinson-White syndrome?
In WPW, the heart has an extra electrical pathway that causes a rapid heartbeat (tachycardia). It forms before birth as the heart is developing. It's unclear why the extra electrical pathway forms. It sometimes occurs with other congenital heart defects. A few people with WPW have a gene defect that is passed down through the family.
Who is at risk for Wolff-Parkinson-White syndrome?
WPW affects both men and women. In most cases, the cause of WPW isn’t known. But researchers have identified gene mutations that may be responsible for the disorder in a few people.
What are the symptoms of Wolff-Parkinson-White syndrome?
With WPW, you may not have any episodes of tachycardia for many years. Symptoms may also start and stop suddenly and occur at any age. Typical symptoms include:
- Shortness of breath
- A pounding in your chest
- Dizziness
- Passing out or fainting
- Chest pain
- Cardiac arrest and death (rare)
How is Wolff-Parkinson-White syndrome diagnosed?
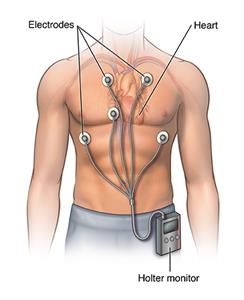
The characteristic finding in WPW is pre-excitation or a delta wave on a test called an electrocardiogram (ECG). The ECG measures the electrical activity in your heart and your heart rate. When a delta wave is present on the ECG, it means that there is an extra pathway conducting electricity from the atria to the ventricles. This extra pathway gets the ventricles to act earlier than normal. This creates the abnormality. Sometimes this is seen on an ECG without any symptoms. If you have symptoms of tachycardia that come and go, your healthcare provider will likely do an ECG. WPW syndrome is diagnosed when this WPW pattern is seen on ECG and you have symptoms or documentation of an arrhythmia involving this extra pathway. Other tests may include:
- Conducting an ECG as you walk on a treadmill (stress test)
- Wearing a type of recorder, called a Holter monitor, that records an ECG for 24 to 48 hours, or longer
- Wearing a type of recorder, called an event recorder, that records your heart rate and rhythm over a few weeks.
- Electrophysiologic testing, a procedure that involves threading catheters into your heart through a vein in your groin to evaluate the heart's electrical system.
How is Wolff-Parkinson-White syndrome treated?
You may not need any treatment if you don't have symptoms. Or if you have infrequent symptoms. Also, symptoms sometimes go away as people get older. If you do need treatment, there are many choices:
- You may be able to stop an episode of tachycardia by massaging your neck over the carotid artery. (Check with your healthcare provider to make sure it is safe for you to do this. And never massage both sides at the same time.) You can also try coughing, or bearing down like you are having a bowel movement. This is called a Valsalva maneuver.
- You may be able to take medicine to stop or prevent tachycardia. But there is no medicine that will cure this condition. Medicines can make the tachycardia worse in rare cases. This is the case when someone is in atrial fibrillation and they also have WPW.
- If medicine and the Valsalva maneuver don't work to stop sustained arrhythmia, you may need to go to the hospital for cardioversion. This procedure restores your heartbeat to a normal rhythm by passing an electric current through your chest into your heart.
- If you are having frequent or uncontrolled episodes of tachycardia, you may have a procedure called catheter ablation. Your healthcare provider threads a long, thin, flexible tube (catheter) through a vein in your groin to the heart. There, low-voltage, high-frequency electrical energy or cold therapy is used to destroy the abnormal connection. The treatment cures WPW about 90% of the time.
What are possible complications of Wolff-Parkinson-White syndrome?
WPW is not often a major problem for most people. You can manage or correct the condition with treatment. Worrisome symptoms include fainting with very rapid heart rates. There is a very small risk of cardiac arrest and death if the heart rate becomes extremely rapid. This may be seen in people who also have atrial fibrillation (another type of arrhythmia).
How can I manage Wolff-Parkinson-White syndrome?
There is no way to prevent WPW. But you can prevent complications by learning as much as you can about the disease. Work closely with your cardiologist (healthcare provider who specializes in diseases of the heart) to find the best treatment. Ask them to teach you how to do a Valsalva maneuver.
Here are some helpful lifestyle suggestions:
-
Don't smoke.
-
Work with your healthcare provider to keep conditions like high cholesterol and high blood pressure under control.
-
Eat a heart-healthy diet.
-
Maintain a healthy weight.
-
Get regular exercise.
- Manage stress.
-
Tell your healthcare provider right away if you have symptoms of WPW.
Key points about Wolff-Parkinson-White syndrome
- Wolff-Parkinson-White syndrome is a type of heart condition that you are born with. It causes a fast heart rate.
- Medicine can help control symptoms.
- Cardiac ablation can cure the disease in most cases.
- Talk with your healthcare provider right away if you have symptoms of WPW.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions, especially after office hours or on weekends.