Relapsing-Remitting Multiple Sclerosis
What is relapsing-remitting multiple sclerosis?
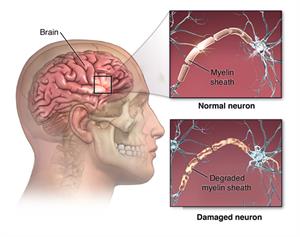
In multiple sclerosis (MS), the central nervous system, which includes the brain and spinal cord, becomes damaged. MS causes the immune system to attack the myelin, which is the insulation protecting the nerves. The nerves themselves can also be damaged. When myelin or the nerves become damaged, nerves can't correctly pass along their signals. The damaging process forms scar tissue called sclerosis, which gives the disease its name of multiple sclerosis.
Different types of MS affect people in different ways. One type is called relapsing-remitting MS. With this type, you have flare-ups of the disease, or relapses. Between these flare-ups, you have periods of recovery, or remissions. During a remission, all symptoms may not improve completely. This leads to symptoms getting worse with each flare-up.
Most people diagnosed with MS start off with the relapsing-remitting type. In most cases, the course of the disease changes after a few decades and is then likely to become steadily worse.
MS most often develops in people in their 20s and 30s. Women are twice as likely to have MS as men.
What causes relapsing-remitting MS?
MS occurs when your body’s immune system attacks the central nervous system, damaging the myelin that protects nerve fibers. Experts believe that environmental factors trigger the disease in people whose genetics make them susceptible to MS.
Who is at risk for relapsing-remitting MS?
-
Scientists think MS may be caused by an infection that lays dormant in the body, such as Epstein-Barr Virus (the virus that causes infectious mononucleosis).
-
Scientists also think there may be a genetic susceptibility for some people.
-
Cigarette smoking appears to increase risk.
What are the symptoms of relapsing-remitting MS?
These are often the earliest symptoms of MS:
-
Trouble seeing
-
Sensitivity to heat
-
Numbness, especially in the feet
-
Weakness
-
Severe tiredness (fatigue)
-
Trouble thinking clearly
-
Depression
-
Needing to urinate urgently
-
Trouble with balance
-
Lack of coordination
Relapsing-remitting MS is marked by relapses that last at least 24 hours. During a relapse, symptoms get worse. A relapse will be followed by a remission. During a remission, symptoms partly or completely go away.
How is relapsing-remitting MS diagnosed?
Healthcare providers use many tests to help diagnose MS. Your healthcare provider will ask you questions about your symptoms. It's important to rule out other diseases that can cause similar symptoms.
Your healthcare provider will also check to see how well your vision, your sense of balance, and other functions are working. You will need an MRI of your brain and spine. This may find areas of damage in your brain or spinal cord that suggest you may have MS.
Another possible test measures what’s called visual evoked potentials. Painless electrodes placed on your scalp measure how your brain responds to things you see.
Your healthcare provider may want to check your blood for other signs of disease. They may also order a test called a spinal tap (lumbar puncture) to look at a sample of your spinal fluid.
How is relapsing-remitting MS treated?
MS is not considered curable. But different types of medicine are available to decrease inflammation and slow down the progression of the disease. These medicines include:
-
Beta-interferon
-
Glatiramer acetate
-
Monoclonal antibodies
-
Dimethyl fumarate
-
Fingolimod
-
Teriflunomide
-
Mitoxantrone
- cladribine
Other medicines can be prescribed to treat:
-
Muscle spasms
-
Urge to urinate
-
Depression
-
Erectile dysfunction
-
Fatigue
Your healthcare provider may also suggest steroids to reduce symptoms during flare-ups. If steroids are not effective, your provider may advise plasmapheresis, a blood-cleansing procedure.
What are possible complications of relapsing-remitting MS?
In most cases, relapsing-remitting MS is mild. But you may need to use a cane or other mobility device. In some cases, the disease is severe and makes you unable to care for yourself. Seldom does it cause death.
Living with relapsing-remitting MS
If you have relapsing-remitting MS, you can take steps to manage your condition.
-
Physical therapy may help relieve muscle spasms.
-
Eat a diet low in saturated fat and trans fat. Eat more foods with healthy omega-3 fatty acids because these nutrients are believed to fight inflammation.
-
Talk with a counselor to help with depression.
-
Stay away from situations that cause you to become overheated.
-
Don't smoke.
-
Get a moderate amount of exercise and enough sleep.
Key points about relapsing-remitting MS
-
MS most often develops in people in their 20s and 30s.
-
MS affects the way your muscles and eyes work.
-
Although there is no cure, medicines can help you manage your symptoms.
-
Adopting a healthy lifestyle can also help you manage your disease.
-
Preventing overheating or other triggers can prevent flares of MS.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your provider tells you.
-
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
-
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if you do not take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your healthcare provider if you have questions.


