University Hospitals Cleveland Medical Center Implants First-in-Human Patient-Specific 3D Printed Tracheal T-tube
July 25, 2024
Patient’s care team received compassionate use from the FDA
Innovations in Pulmonology, Critical Care & Sleep Medicine | Summer 2024
Innovations in Ear, Nose & Throat | Summer 2024
In June 2024, respiratory health specialists at University Hospitals (UH) Cleveland Medical Center placed the first-ever patient-specific 3D printed T-tube into a human patient. The patient had been suffering complications from his commercial grade T-tube. The FDA granted compassionate use for the case.
 N. Scott Howard, MD, MBA
N. Scott Howard, MD, MBA Benjamin Young, MD
Benjamin Young, MDA tracheal T-tube is shaped like the letter “T” and made of silicone. It lets patients breathe through an opening in their neck instead of through their mouth. It can be used for many reasons, including creating an upper airway for a person who may have damage to that area. T-tubes come in several sizes but are not created to fit an individual person’s unique anatomy. Sometimes the fit of a commercial T-tube can cause complications like mucus plugging, granulation tissue formation, interference with the vocal cords, and serious airway blockages.
Sterling Brown received a tracheostomy in September of 2022 when he was admitted to the hospital for life-threatening complications from obesity and high blood pressure.
“Sterling has a very uniquely shaped airway,” said N. Scott Howard, MD, MBA, otolaryngologist and Director of the Voice, Airway and Swallowing Center at UH Cleveland Medical Center and UH Ear, Nose & Throat Institute, and Associate Professor at Case Western Reserve University School of Medicine. “The commercially available T-tube wasn’t a good fit for him despite attempts to modify it and was causing complications including infections and damage to his vocal cords.”
The FDA has not approved patient-specific 3D printed T-tubes for medical use, but similar patient-specific 3D printed lower airway Y-stents do have FDA approval. A Y-stent is used to relieve obstructions in the lower airways near the lungs when the airway is damaged or diseased. It is used to support the lower airway when other techniques fail. Benjamin Young, MD, Medical Director of Bronchoscopy at UH Cleveland Medical Center, and Associate Professor at the School of Medicine, has extensive experience with 3D printed Y-stents.
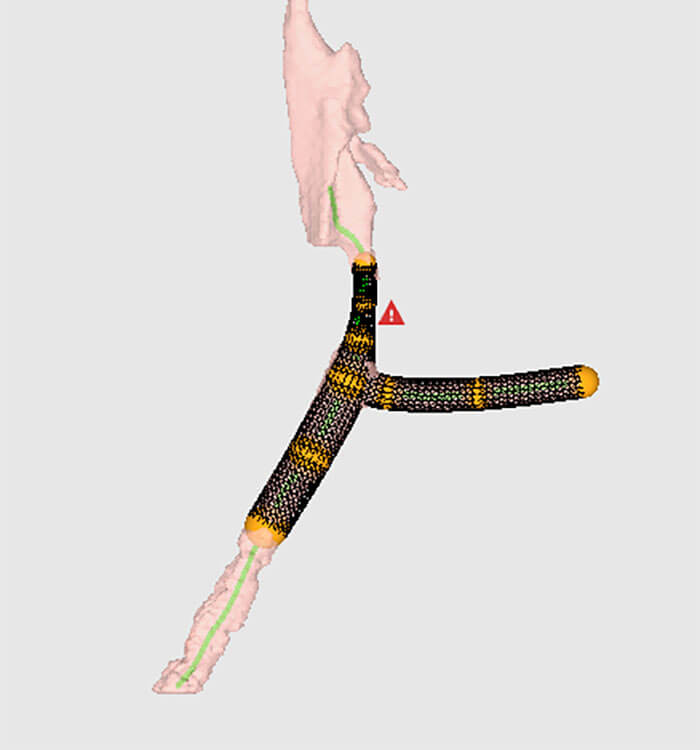 VisionAir T-tube.
VisionAir T-tube.“We’ve had success using the custom airway Y-stents in several of our patients,” said Dr. Young. “When it became apparent Sterling’s T-tube was causing so much trouble for him, we believed a custom device might help if we could make it happen.”
Dr. Howard applied for and received compassionate use approval from the FDA for a patient-specific T-tube. He worked with VisionAir Solutions, a Cleveland based medical device company that specializes in patient-specific silicone airway stents. The company’s software uses a CT scan to create a 3D model of the airway. Dr. Howard and Dr. Young tailored the stent design to the exact dimensions and specifications of the airway. In Brown’s case this was done for the first time with a T-tube that protrudes from his tracheostomy and supports the airway above and below the tracheostomy.
Brown, now 36, has a passion for singing and was featured on season 3 of American Idol. He was prevented from singing and even talking for nearly two years because of complications following his illness, prolonged intubation and tracheostomy. His patient-specific T-tube was placed on June 26, 2024.
 UH Pulmonology patient Sterling Brown.
UH Pulmonology patient Sterling Brown.“After the surgery to place this T-tube, which was made for me, I had fewer complications,” said Brown. “The fit is improved, and it creates less mucus. I’m talking better and the tube is no longer damaging my vocal cords.”
“Sterling’s case was extremely complicated,” said Dr. Howard. “At UH, we have a world class team, our Complex Airway Team, with multiple subspecialists to help us collectively manage these patients and give them a better quality of life.”
Traditional T-tubes need to be changed out periodically and Brown’s patient-specific version will too, but he can now go longer periods between replacements and revision surgery which means fewer procedures and trips to the hospital.
“I’m grateful to my medical team for not giving up. I’ve been sick for a long time,” he said. “I have hope to live a normal life again and find joy in singing thanks to the determination of my doctors.”
Brown is currently receiving care and therapy in a nursing facility. If he continues to improve, he could eventually have the T-tube removed and use the airway he was born with to breathe, talk, and sing.


